
Microsurgical Anatomy of the Cavernous Sinus
Authors
Talat Kiris, MD
Suresh K. Sankhla, MD
Michael T. Lawton, MD
Joseph M. Zabramski, MD
Robert F. Spetzler, MD
Division of Neurological Surgery, Barrow Neurological Institut, Mercy Healthcare Arizona, Phoenix, Arizona
Abstract
Although the anatomy of the cavernous sinus is complex, detailed knowledge of this area is essential for safe surgical approaches to the region. Ten cadaveric dissections were therefore performed to examine the microsurgical anatomy of the cavernous sinus. Relevant dural, arterial, venous and cranial nerve anatomy is presented. The anatomical triangles that define routes of access into the cavernous sinus as well as various surgical approaches commonly used in the management of lesions of the cavernous sinus are reviewed.
Key Words : anatomy, cavernous sinus, cranial nerves, internal carotid artery
Surgery in the cavernous sinus was long associated with a significant risk of complications. Consequently, this area was considered a “no man’s land” for direct surgical intervention. Inadequate knowledge of the anatomy and a lack of microsurgical techniques were the major reasons responsible for the inability to treat lesions in thisarea effectively. In 1965 Parkinson34 first described a direct surgical approach to the cavernous sinus for a carotid-cavernous fistula. This pioneering work renewed interest in the surgical management of cavernous sinus lesions. Subsequent microanatomical studies2,17,24,35,39,40,44,48 and surgical series1,3,6,7,9-11,14,16,18-20,29-33,45 have demonstrated that direct approaches to cavernous sinus lesions can be performed safely and effectively.
Detailed knowledge of the anatomy of the cavernous sinus is essential for safe surgical approaches to the region. The microscopic anatomy of the cavernous sinus was therefore examined in 10 dissections (5 in cadaveric specimens). The surgically relevant anatomy is reviewed.
Cavernous Sinus and Its Coverings
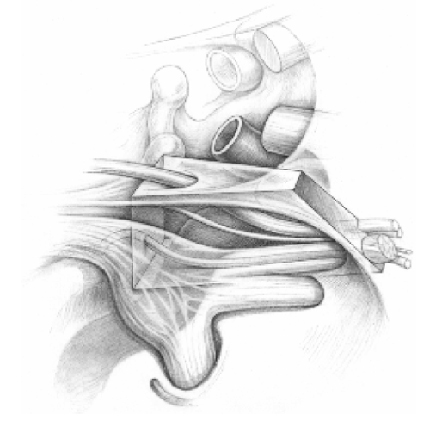
Although previously described as a tetrahedron6 or a pentahedron,16 in our dissections the cavernous sinus appeared as a hexahedron-shaped space on either side of the sella turcica at the convergence of the floors of the anterior and middle cranial fossae, the sphenoid wing, and petroclival ridge (Fig. 1). The margins of this compartment are limited by the medial aspect and lesser and greater wing of the sphenoid bone, the anterior and posterior clinoids, and the tip of the petrous pyramid. The average dimensions of the cavernous sinus are 2 cm long by 1 cm wide. It is bounded on all sides by dura mater, which is continuous from the base of the middle and posterior cranial fossae and the diverging aspects of the tentorium.26,35,49 The floor and medial wall of the cavernous sinus are formed by a periosteal layer of dura. As it continues upward along the lateral surface of the pituitary gland and clinoid processes, this thin layer is joined by another layer of dura that covers the floor of the sella turcica. The double-layered dura of the clivus extends anteriorly to form part of the posterior wall. The double-layered dura of the floor of the middle fossa extends medially at the superior border of the second division of the fifth cranial nerve to become the lateral wall of the cavernous sinus.
The roof of the cavernous sinus is formed by the upward extension of the lateral wall as it joins with the thickened tentorial edge attached to both the posterior and the anterior clinoid processes. Medially, the roof is continuous with the diaphragm sella. Anteriorly, the cavernous sinus tapers and twists to terminate at the superior orbital fissure. Posterosuperiorly, it ends at the tentorium. Posteromedially, the compartment is continuous with the lateral edge of the clivus, and inferolaterally it extends into a funnel-shaped space around the internal carotid artery (ICA) through the foramen lacerum.
The structures lying within the cavernous sinus are the ICA and its branches, the abducent nerve, sympathetic nerve fibers, and fat. The oculomotor and trochlear nerves and the first and second divisions of the trigeminal nerve course within the lateral wall of the sinus.
The morphological structure of the cavernous sinus is controversial. Some studies interpret the structure as a trabeculated intradural venous channel.2,17 Other studies have interpreted the cavernous sinus as a plexiform network of veins.34,35,48,49 Microanatomical dissections of fetal cavernous sinuses by Knosp et al.23 showed that this area was composed of a network of veins separated and surrounded by loose connective tissue.
Intracavernous Course of ICA
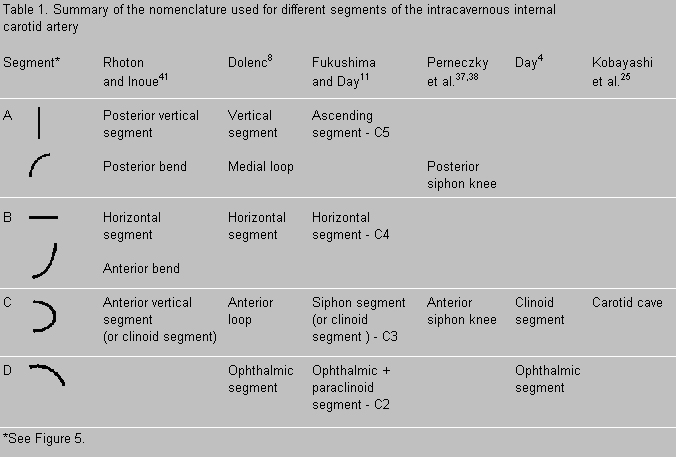
The ICA runs diagonally through the base of the skull extradurally, measuring approximately 6 cm along its intrapetrous and intracavernous course.8 From the point of its entry at the skull base to its exit into the subarachnoid space, the ICA courses laterally to medially in the coronal plane, posteriorly to anteriorly in the sagittal plane, and inferiorly to superiorly in the axial plane. The ICA is divided into four segments (two horizontal and two vertical) and four loops (posterior, lateral, medial and anterior, Fig. 2). Both the intrapetrous and intracavernous portions of the ICA have a horizontal and a vertical segment.
The intracranial course of the ICA begins with its intrapetrous vertical segment. The junction of this segment with the intrapetrous horizontal segment forms the posterior loop, which is completely surrounded by petrous bone. Within the carotid canal the ICA is surrounded by connective tissue and a periosteal lining. The horizontal segment of the intrapetrous ICA is also surrounded by a periarterial venous plexus. Although the artery can easily be separated from the periosteal lining during surgery, care must be taken to avoid inducing venous bleeding from the periarterial venous plexus. This segment of the ICA gives rise to variant branches, including the vidian artery, the caroticotympanic artery, and the periosteal arteries. In certain occlusions of the cervical carotid artery, the antegrade progression of the thrombus may be prevented and the patency of the intrapetrous segment of the ICA may be maintained by retrograde anastomotic flow through the branches in this region.36
This portion of the artery is close to the geniculate ganglion, lesser and greater superficial petrosal nerves, cochlea, tensor tympani muscle, and eustachian tube. The geniculate ganglion lies posterolateral to the posterior loop. The greater superficial petrosal nerve lies above and parallel to the horizontal petrosal ICA. The lesser superficial petrosal nerve is lateral to the greater superficial petrosal nerve. Both nerves originate from the geniculate ganglion. The cochlea is located posterosuperior to the posterior loop, and the eustachian tube and tensor tympani muscle are located lateral and parallel to the horizontal segment of intrapetrosal ICA. Both the foramen ovale and foramen spinosum are anterolateral to where the horizontal intrapetrosal ICA exits from the carotid canal. The foramen ovale lies more anteriorly than the foramen spinosum, which assumes a more lateral position.
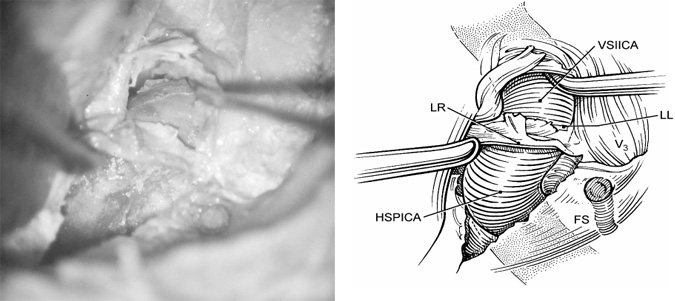
The junction of the intrapetrous horizontal and intracavernous vertical portions of the ICA forms the lateral loop that overlies the foramen lacerum and runs below the lower aspect of the third division of the trigeminal nerve. At its exit from the bone, the artery is fixed by a thick fibrous band of dura known as the lateral ring (Fig. 3). After passing through the lateral ring, the artery runs under the trigeminal nerve—in most cases without a bony cover.17 The intracavernous vertical segment is the initial ascending portion of the ICA immediately distal to the foramen lacerum. The medial loop is formed at the junction of the intracavernous vertical and horizontal segments of the ICA. The medial loop is situated adjacent to the lateral aspect of posterior clinoid process. The intracavernous horizontal segment of the ICA runs forward toward the anterior portion of the cavernous sinus where it curves upward (anterior loop) before exiting through the roof of the cavernous sinus (Fig. 2). This portion of the ICA (clinoidal segment) lies medial and inferior to the anterior clinoid process. A small recess situated medial to the clinoidal segment of the ICA is called the carotid cave.25
The ICA is surrounded by two rings at this zone of dural transition (Fig. 4). The first ring (proximal ring or carotico-oculomotor membrane) is formed by a thin protective layer of dura that lies between the anterior clinoid process and the third cranial nerve. The second ring (distal or dural ring) is composed of strong strands of connective tissue that attach the artery in a radiating arrangement to the planum sphenoidale, diaphragma sella, and anterior clinoid process. The plane of the distal ring is oblique, and the ring is thicker laterally and thinner on its medial surface. The segment of the ICA between these two rings, the clinoidal segment, is approximately 5 mm long. This ring must be divided sharply during surgery to expose the clinoidal segment. The loose layer around the artery allows blunt dissection, and working lateral and anterior to the artery in this plane permits an adequate exposure of the anterior loop without disrupting the venous plexus of the cavernous sinus.
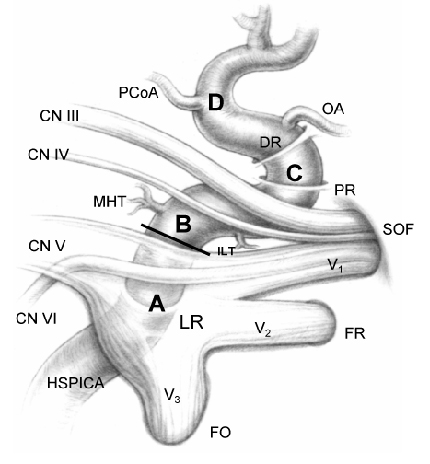
The risk of injury to the venous plexus is significantly higher if dissection continues further down along the anterior loop across the carotico-oculomotor membrane.24,38 The branches of the ophthalmic segment usually originate just beyond the distal ring. The ophthalmic artery originates superomedially, whereas the superior hypophyseal artery exits more inferomedially.4 Different authors have applied different nomenclature to the various segments of the cavernous ICA (Fig. 5, Table 1).
Branches of the Intracavernous ICA
The origin and course of the branches of the intracavernous portion of the ICA exhibit considerable variations.18 The meningohypophyseal trunk and the inferolateral trunk are the most consistent branches. They form important surgical landmarks, and trauma to these branches can generate pseudoaneurysms or carotid-cavernous fistulae.
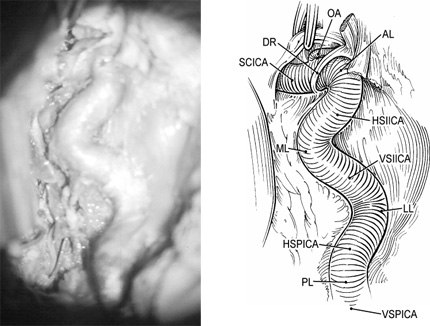
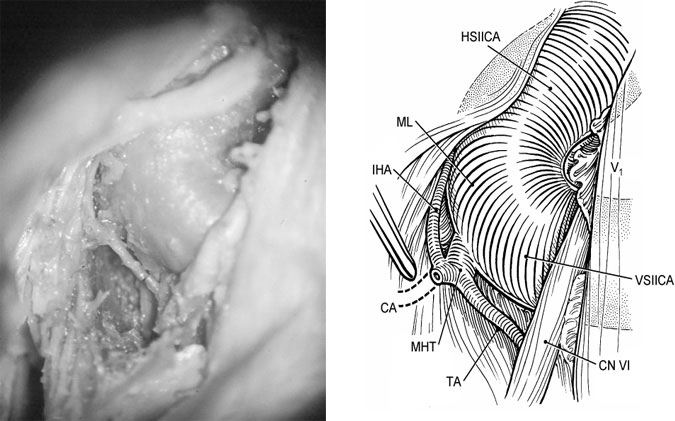
The meningohypophyseal trunk (truncus caroticocavernosus posterior) is the largest and the most proximal branch of the intracavernous ICA (Fig. 6). It originates from the medial loop and is always medial to the sixth cranial nerve where it crosses the vertical segment of the ICA. The meningohypophyseal trunk gives rise to three branches.8, 17, 22, 34 First, the tentorial artery or artery of Bernasconi-Cassinari, is the most constant branch of the trunk and supplies the tentorium. Second, the inferior hypophyseal artery anastomoses with the opposite inferior hypophyseal artery and supplies the posterior lobe of the pituitary and the dura of the sellar floor. Third, the clival, or dorsal meningeal artery, divides into medial and lateral branches that supply the superior clival dura and the sixth cranial nerve within Dorello’s canal, respectively.
The inferolateral trunk (artery of inferior cavernous sinus, truncus caroticocavernosus lateralis) is the second most constant branch. This artery arises from the inferior and lateral side of the midportion of the intracavernous horizontal segment approximately 5 to 8 mm distal to the origin of the meningohypophyseal trunk. It typically divides into four branches.22 The anteromedial branch runs toward the superior orbital fissure and supplies the third, fourth and sixth cranial nerves as well as the ophthalmic division of the trigeminal nerve. The anterolateral branch accompanies the maxillary branch of the trigeminal nerve through the foramen rotundum and anastomoses with branches of the internal maxillary artery. The posterior branch courses with the mandibular branch of the trigeminal nerve through the foramen ovale and anastomoses with the internal maxillary artery and/or petrosal branch of the middle meningeal artery. Finally, the superior branch runs adjacent to and supplies the fourth cranial nerve. When the tentorial branch of the meningohypophyseal artery is absent, the tentorium is supplied by a branch of the inferolateral trunk called the marginal tentorial artery.18
The capsular artery of McConnell arises from the medial aspect of the horizontal segment and supplies the dura of the sellar floor, the anterior sellar wall, and the capsule of the pituitary gland. Other variabilities in the vascular anatomy of this region include a persistent trigeminal artery; the intracavernous origin of the ophthalmic artery; and an accessory, hypoplastic ophthalmic artery.18
Venous Anatomy
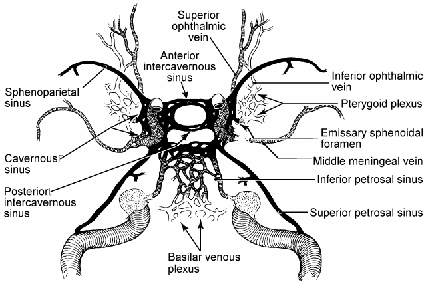
The cavernous sinuses have extensive venous connections with the face, eyes, orbit, nasopharynx, mastoid, middle ear, cerebrum, cerebellum, and brain stem (Fig. 7).12 Each cavernous sinus receives blood mainly from the superior and inferior ophthalmic veins. The superior ophthalmic vein passes through the superior orbital fissure and joins the cavernous sinus, whereas the inferior orbital vein may either connect to the cavernous sinus separately or join the superior ophthalmic vein before entering the sinus.33 Each cavernous sinus is also connected to the retina through the central retinal vein, to the nasopharynx by the emissary veins from the pterygoid venous plexus, to the cerebral hemispheres by the superficial middle cerebral (Sylvian) vein, and to the dura by the middle meningeal vein.12 Furthermore, both cavernous sinuses are fed by the sphenoparietal sinuses and the intercavernous sinuses. The main drainage of the cavernous sinuses is through the superior petrosal sinus to the junction of the transverse and sigmoid sinuses and through the inferior petrosal sinus to the jugular bulb and internal jugular vein.
Harris and Rhoton17 described four venous spaces in the cavernous sinus that were named on the basis of their relationship to the intracavernous ICA: medial, lateral, anterior-inferior and posterior-superior. The medial and lateral spaces are located between the ICA and the medial and lateral walls. The posterior-superior space is confined between the ICA and the roof of the cavernous sinus. The anterior-inferior space is situated in the concavity below the medial loop of cavernous ICA. Lang and Kageyama27 and Sadasivan et al.42 described a fifth space, namely, the anterior cavernous space anterior to the anterior loop of the ICA. However, the presence of this space depends on the tortuosity and shape of the intracavernous ICA and can overlap with the anterior-inferior space.
Cranial Nerves
The relationships of the various cranial nerves to the cavernous sinus have been somewhat controversial. Our own dissections and the majority of published reports confirm that the abducent nerve, along with the ICA and its associated sympathetic plexus, travels through the cavernous sinus proper. In contrast, the oculomotor and trochlear nerves as well as the ophthalmic and maxillary branches of the trigeminal nerve pass between the superficial and deep layers of the lateral cavernous sinus wall.8, 17,18, 34, 35, 37, 44, 50 Umansky and Nathan50 demonstrated that these two layers of the cavernous sinus wall can be readily separated. These authors noted that the inner layer includes the sheaths that surround the cranial nerves after they penetrate the sinus wall. A reticular membrane extends between the sheaths of the cranial nerves, thus completing the deep layer. The reticular membrane is often incomplete, particularly between the sheaths of the oculomotor and trochlear nerves as well as the ophthalmic division of the trigeminal nerve. This area of the lateral wall is quite thin and transparent and is therefore easily recognized as the triangular space defined by Parkinson.34
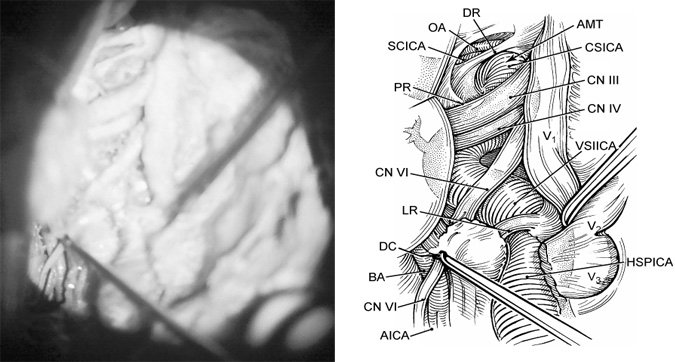
The third and fourth cranial nerves enter the sinus superiorly, whereas the fifth and sixth cranial nerves pierce the wall of the sinus posteroinferiorly (Fig. 4). The third cranial nerve, after entering the roof of the cavernous sinus lateral to the posterior clinoid process, runs in the deep layer of the lateral wall and lies immediately under the lower margin of the anterior clinoid process before it exits the sinus to enter the superior orbital fissure (Fig. 8). In this region, the third cranial nerve is separated from the anterior clinoid process by a thin layer of dura and can easily be injured during drilling and removal of the anterior clinoid process.18 The thin dural layer, however, extends further around the ICA to form the proximal ring, as mentioned earlier.
The fourth cranial nerve enters the roof of the cavernous sinus posterolateral to the third cranial nerve and under the free edge of the tentorium. Within the deep layer of the lateral wall, it travels almost parallel to the longitudinal axis of the horizontal segment of the ICA and then passes over the third cranial nerve to exit through the superior orbital fissure (Figs. 4 and 9).
The ophthalmic division of the fifth cranial nerve runs within the deep layer of the lateral wall of the cavernous sinus in its lower portion and courses obliquely upward to exit the sinus through the superior orbital fissure. The maxillary division is situated at the most posteroinferior aspect of the lateral wall and leaves the cranium through the foramen rotundum, following a more horizontal course than the first division. The mandibular division does not enter the cavernous sinus and exits the cranium through the foramen ovale after passing over the lateral loop of the ICA. The Gasserian ganglion is located outside the cavernous sinus in Meckel’s cave, which is a concavity at the apex of the petrous bone formed by the extension of the meninges from the posterior fossa along the fifth cranial nerve (Figs. 8 and 9).
The sixth cranial nerve enters the sinus through Dorello’s canal, which is defined by the petroclival ligament (Gruber’s ligament) superiorly and by the petrous apex inferiorly. The sixth nerve is fixed to the dura at its point of entry but courses freely within the cavernous sinus. It traverses the vertical segment of the intracavernous ICA medially to laterally and runs parallel to the horizontal segment underneath the ophthalmic division of the trigeminal nerve to reach the superior orbital fissure (Fig. 4). In the cavernous sinus, the sixth cranial nerve frequently splits into multiple rootlets.17
The sympathetic nerve fibers that form the plexus surrounding the ICA join the sixth cranial nerve as it passes over the ICA within the cavernous sinus. The majority of fibers travel a few millimeters with the sixth cranial nerve before joining the ophthalmic division of the trigeminal nerve immediately before it enters the superior orbital fissure. Approximately 30% of the fibers continue with the sixth cranial nerve as it enters the orbit.43, 52
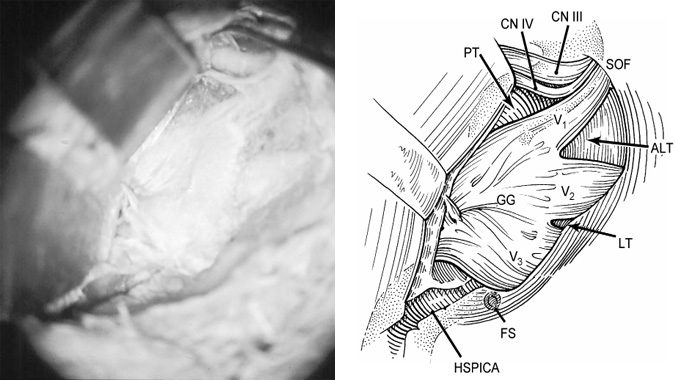
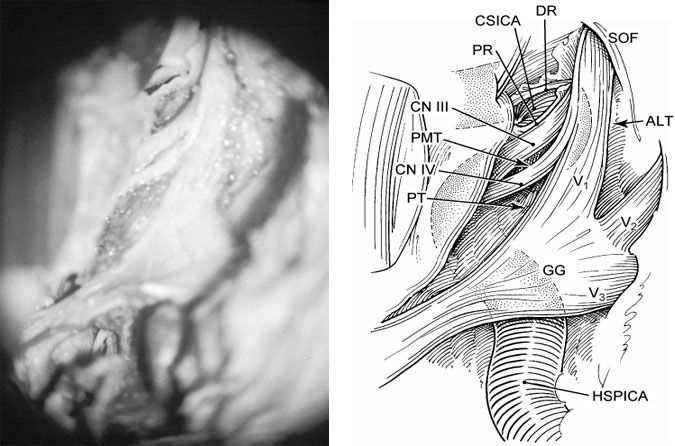
Figure 9. Cadaveric photograph (A) and illustration (B) showing the inferolateral view of the cavernous sinus region. The Gasserian ganglion (GG) and its branches are visible after the superficial layer of the lateral wall of the cavernous sinus and the dura of Meckel’s cave have been removed. CN III, oculomotor nerve; CN IV, trochlear nerve; V1, ophthalmic division of trigeminal nerve; V2, maxillary division of trigeminal nerve; V3, mandibular division of trigeminal nerve; ALT, anterolateral triangle; LT, lateral triangle; FS, foramen spinosum with sectioned middle meningeal artery; HSPICA, horizontal segment of the petrosal internal carotid artery; SOF, superior orbital fissure; and PT, Parkinson’s triangle.
Triangles and Routes of Entry
The points of entry of the cranial nerves are relatively fixed and provide important anatomical landmarks for safe surgical entry into the cavernous sinus. After Parkinson’s initial description of a triangle in the lateral wall of the cavernous sinus,34 a number of other triangles in this region have been described by other authors and are summarized below.5, 8, 11, 13, 16, 21, 31, 51
Anteromedial Triangle
This triangular area is defined by the lateral aspect of the optic nerve, the medial aspect of the third cranial nerve, and the tentorial edge from the entry point of the third cranial nerve to the entry point of the optic nerve into the optic canal (Fig. 4). It contains the clinoid segment of the ICA and is exposed by removing the anterior clinoid process either extradurally or intradurally. This triangle can be enlarged by dissecting the proximal dural ring from the third cranial nerve and incising the dura propria along the longitudinal axis of the optic nerve.
Medial (Hakuba’s) Triangle
This triangle is formed by connecting three points in the superior wall of the cavernous sinus: the lateral margin of the supraclinoid ICA, the dural entrance of the oculomotor nerve, and the anterolateral margin of the posterior clinoid process. Through this window the horizontal portion of the cavernous ICA can be explored.
Paramedian Triangle
The medial and lateral boundaries of this space are defined by the lateral aspect of the third cranial nerve and by the medial aspect of the fourth cranial nerve, respectively (Fig. 8). The posterior margin is the portion of the tentorial edge between the entry points of the third and fourth cranial nerves. This triangle is used to explore the medial loop of the intracavernous ICA and the meningohypophyseal trunk.
Parkinson’s Triangle
This space is limited medially by the lateral aspect of the fourth cranial nerve, laterally by the medial aspect of the ophthalmic division of the trigeminal nerve, and posteriorly by the dural edge between the entry points of these two nerves (Figs. 8 and 9). This triangular area is relatively narrow and can be enlarged by slight retraction of the fourth cranial nerve medially and the ophthalmic division of the trigeminal nerve laterally. The entire intracavernous segment of the ICA from the lateral ring to the proximal ring can be explored through this route. This corridor is also well suited for exposing the complete course of the sixth cranial nerve from its entry through Dorello’s canal to its exit through the superior orbital fissure.
Anterolateral (Mullan’s) Triangle
This triangle is situated between the ophthalmic and maxillary divisions of the trigeminal nerve and the bone of the middle fossa between the foramen rotundum and superior orbital fissure (Figs. 8 and 9). This space is used to expose the superior orbital vein and the sixth cranial nerve and to access carotid-cavernous fistulae.
Lateral Triangle
This area is defined by the maxillary and mandibular divisions of the trigeminal nerve and the bone in the middle fossa between the foramen rotundum and foramen ovale (Fig. 8). Sometimes the sphenoidal emissary foramen and vein can be found in this area, connecting the cavernous sinus with the pterygoid venous plexus. This triangle also may be used to approach masses that extend laterally in the cavernous sinus.
Posterolateral (Glasscock’s) Triangle
This triangle is bounded by the greater superficial petrosal nerve medially, the posterior aspect of the mandibular division of the trigeminal nerve anteriorly, and by a line between the foramen spinosum and the arcuate eminence of the petrous bone posteriorly. The triangle identifies the bone that must be removed to expose the horizontal intrapetrosal segment of the ICA for proximal control or for a bypass graft.47
Posteromedial (Kawase’s) Triangle
First described by Kawase et al.,21 this area is more quadrangular than triangular. The landmarks for this area in the middle fossa are the posterior border of the mandibular division of the trigeminal nerve anteriorly, the arcuate eminence posteriorly, the greater superficial petrosal nerve laterally, and the petrous ridge with the superior petrosal sinus medially. Bone removal in this region enables access to the petroclival area, the anterolateral brain stem, and the vertebrobasilar junction through a corridor between the trigeminal nerve and facial-vestibulocochlear nerve complex.
Inferomedial Triangle
This triangle is defined medially by a line connecting the posterior clinoid process and the sixth cranial nerve at Dorello’s canal, laterally by a line connecting the fourth cranial nerve at the edge of tentorium and the sixth cranial nerve at Dorello’s canal, and by the petrous apex at the base.
Inferolateral Triangle
This triangle is lateral to the inferomedial triangle and is bounded medially by the line between the sixth cranial nerve at Dorello’s canal and the fourth cranial nerve at the edge of the tentorium, laterally by the line connecting the sixth cranial nerve at Dorello’s canal and the petrosal vein at the superior petrosal sinus, and by the petrous apex at the base.
Surgical Approaches
Interest in direct surgical approaches to lesions of the cavernous sinus has grown as neuroradiological imaging and microsurgical technique have improved. A number of different routes to the cavernous sinus have been described, including the subtemporal approach through the lateral wall,6, 31, 34, 37, 44 the pterional approach through the superior wall,14, 38 the transpetrosal-transtentorial approach through the posterior wall,15 the contralateral pterional transsylvian approach through the medial wall,14, 38 and the transsphenoidal approach through the inferior wall.28 Most of these approaches can be broadly classified as either extradural or intradural. Dolenc,7, 8, 10 however, described a combined extradural-intradural approach that has been commonly used for lesions in this region.
Three extradural (inferior, anterolateral, and medial) and two intradural (superior and lateral) approaches are surgically important.44 The inferior extradural approach is used to expose the horizontal segment of the intrapetrous ICA and the junction of the intracavernous and intrapetrous segments. Further exposure of the ICA underlying the Gasserian ganglion and of the posterior part of the cavernous sinus can only be achieved by dividing the mandibular division of the trigeminal nerve or by adopting a more inferior subtemporal-infratemporal approach.45 The anterolateral approach permits extradural access to the floor of the anterior and middle cranial fossae for removal of the anterior clinoid process and the roof of the orbit and optic canal. This approach exposes the entire clinoid segment of the ICA. The medial approach may be utilized to expose the medial venous space, the anterior and medial surfaces of the anterior loop, and the medial surface of the intracavernous horizontal segment through the sphenoid sinus. Via this exposure, it is possible to achieve access to the contralateral cavernous sinus through the sphenoid sinus or around the pituitary gland.46
The intradural superior approach removes the anterior clinoid process and enters the cavernous sinus through the superior wall, either medially or laterally. It provides an excellent view of the anterior loop of the ICA and the anterior parts of the lateral and posterior-superior venous spaces. The lateral approach enters the cavernous sinus through the lateral wall. The lateral surface of the vertical and horizontal segments of the intracavernous ICA, the medial loop, and the lower part of the anterior loop of the ICA are exposed through this approach. The lateral, anterior-inferior, and posterior-superior spaces as well as the cranial nerves in the wall of the cavernous sinus and the intracavernous portion of the sixth cranial nerve are also exposed. The origins of the meningohypophyseal trunk and the inferolateral trunk can also be visualized.
Optimal exposure of all regions of the cavernous sinus is impossible through a single approach while maintaining proximal and distal control of the intracavernous ICA. A combination of extradural and intradural approaches provides generous exposure of this area and different working angles through the various triangles. Proximal and distal control of the intracavernous ICA ensures safe surgical intervention and also provides the exposure needed to perform a venous bypass from the petrous to the supraclinoid ICA, if necessary. An orbitozygomatic-frontotemporal craniotomy increases extradural and intradural exposure and helps minimize brain retraction.16, 29
Despite advances in neuroimaging, neuroanesthesia, and microsurgical techniques, complications (cranial nerve injuries, cerebrovascular complications, and cerebrospinal fluid leakage) associated with direct operative procedures in the cavernous sinus region still remain high.3 New forms of therapy, such as stereotactic radiosurgery, endovascular techniques, and medical therapy in certain tumors (e.g., bromocriptine for treatment of prolactinomas) provide alternatives for the management of these lesions. The indications of direct operative procedures thus remain a matter of debate. When direct surgical intervention in the cavernous sinus is contemplated, it is important to consider the anatomical location, the pathology of the lesion, the likelihood of achieving a cure, and the risk of operative complications. Every case should be evaluated on an individual basis, weighing such factors as the patient’s age and medical condition and the severity of the disease.
The strategy of combined surgical approaches and multimodality therapy, when appropriate, constitutes the main armamentarium for the management of lesions in and around the cavernous sinus. Conservative management of extensive and incurable tumors, including meningiomas, has been the general trend because of the inability to resect these lesions completely without damaging the cranial nerves. The surgeon’s judgment and the patient’s informed preferences remain the most important factors in planning management strategies for lesions in the cavernous sinus.
References
- Al-Mefty O, Smith RR: Surgery of tumors invading the cavernous sinus. Surg Neurol 30:370-381, 1988
- Bedford MA: The “cavernous” sinus. Br J Ophthalmol 50:41-46, 1966
- Cusimano MD, Sekhar LN, Sen CN, et al: The results of surgery for benign tumors of the cavernous sinus. Neurosurgery 37:1-10, 1995
- Day AL: Aneurysms of the ophthalmic segment. A clinical and anatomical analysis. J Neurosurg 72:677-691, 1990
- Day JD, Fukushima T, Giannotta SL: Microanatomical study of the extradural middle fossa approach to the petroclival and posterior cavernous sinus region: Description of the rhomboid construct. Neurosurgery 34:1009-1016, 1994
- Dolenc VV: Direct microsurgical repair of intracavernous vascular lesions. J Neurosurg 58:824-831, 1983
- Dolenc VV: A combined epi- and subdural direct approach to carotid-ophthalmic artery aneurysms. J Neurosurg 62:667-672, 1985
- Dolenc VV: Intracavernous carotid artery aneurysms, in Carter LP, Spetzler RF, Hamilton MG (eds): Neurovascular Surgery. New York: McGraw-Hill, 1995, pp 629-672
- Dolenc VV, Kregar T, Ferluga M, et al: Treatment of tumors invading the cavernous sinus, in Dolenc VV (ed): The Cavernous Sinus. A Multidisciplinary Approach to Vascular and Tumorous Lesions. New York: Springer-Verlag, 1987, pp 377-391
- Dolenc VV, Skrap M, Sustersic J, et al: A transcavernous-transsellar approach to the basilar tip aneurysms. Br J Neurosurg 1:251-259, 1987
- Fukushima T, Day JD: Surgical management of tumors involving the cavernous sinus, in Schmidek HH, Sweet WH (eds):Operative Neurosurgical Techniques. Philadelphia: W. B. Saunders, 1995, pp 493-510
- Gasecki AP, Barnett HJM: Venous anatomy, in Carter LP, Spetzler RF, Hamilton MG (eds): Neurovascular Surgery. New York: McGraw-Hill, 1995, pp 35-64
- Glasscock ME, III: Exposure of the intra-petrous portion of the carotid artery, in Hamberger CA, Wersall J (eds): Disorders of the Skull Base Region. Proceedings of the Tenth Nobel Symposium. Stockholm: Almqvist & Wicksell, 1969, pp 135-143
- Hakuba A, Matsuoka Y, Suzuki T, et al: Direct approaches to vascular lesions in the cavernous sinus via the medial triangle, in Dolenc VV (ed): The Cavernous Sinus. A Multidisciplinary Approach to Vascular and Tumorous Lesions. New York: Springer-Verlag, 1987, pp 272-284
- Hakuba A, Nishimura S, Jang BJ: A combined retroauricular and preauricular transpetrosal-transtentorial approach to clivus meningiomas. Surg Neurol 30:108-116, 1988
- Hakuba A, Tanaka K, Suzuki T, et al: A combined orbitozygomatic infratemporal epidural and subdural approach for lesions involving the entire cavernous sinus. J Neurosurg 71:699-704, 1989
- Harris FS, Rhoton AL: Anatomy of the cavernous sinus. A microsurgical study. J Neurosurg 45:169-180, 1976
- Inoue T, Rhoton AL, Jr., Theele D, et al: Surgical approaches to the cavernous sinus: A microsurgical study. Neurosurgery 26:903-932, 1990
- Isamat F, Ferrer E, Twose J: Direct intracavernous obliteration of high-flow carotid-cavernous fistulas. J Neurosurg 65:770-775, 1986|}
- Johnston I: Direct surgical treatment of bilateral intracavernous internal carotid artery aneurysms. Case report. J Neurosurg 51:98-102, 1979
- Kawase T, Toya S, Shiobara R, et al: Transpetrosal approach for aneurysms of the lower basilar artery. J Neurosurg 63:857-861, 1985
- Knosp E, Müller G, Perneczky A: The blood supply of the cranial nerves in the lateral wall of the cavernous sinus, in Dolenc VV (ed): The Cavernous Sinus. A Multidisciplinary Approach to Vascular and Tumorous Lesions. New York: Springer-Verlag, 1987, pp 67-80
- Knosp E, Müller G, Perneczky A: Anatomical remarks on the fetal cavernous sinus and on the veins of the middle cranial fossa, in Dolenc VV (ed): The Cavernous Sinus. A Multidisciplinary Approach to Vascular and Tumorous Lesions. New York: Springer-Verlag, 1987, pp 104-116
- Knosp E, Müller G, Perneczky A: The paraclinoid carotid artery: Anatomical aspects of a microneurosurgical approach.Neurosurgery 22:896-901, 1988
- Kobayashi S, Kyoshima K, Gibo H, et al: Carotid cave aneurysms of the internal carotid artery. J Neurosurg 70:216-221, 1989
- Lang J: The anterior and middle cranial fossae including the cavernous sinus and orbit, in Sekhar LN, Janecka IP (eds): Surgery of Cranial Base Tumors. New York: Raven Press, 1993, pp 99-121
- Lang J, Kageyama I: Clinical anatomy of the blood spaces and blood vessels surrounding the siphon of the internal carotid artery.Acta Anat (Basel) 139:320-325, 1990
- Laws ER, Jr., Onofrio BM, Pearson BW, et al: Successful management of bilateral carotid-cavernous fistulae with a trans-sphenoidal approach. Neurosurgery 4:162-167, 1979
- Lesoin F, Pellerin P, Autricque A, et al: The direct microsurgical approach to intracavernous tumors, in Dolenc VV (ed): The Cavernous Sinus. A Multidisciplinary Approach to Vascular and Tumorous Lesions. New York: Springer-Verlag, 1987, pp 323-331
- Morrison G, Hegarty WM, Braush CC, et al: Direct surgical obliteration of a persistent trigeminal artery aneurysm. Case report. J Neurosurg 40:249-251, 1974
- Mullan S: Treatment of carotid-cavernous fistulas by cavernous sinus occlusion. J Neurosurg 50:131-144, 1979
- Natori Y, Rhoton AL, Jr. Microsurgical anatomy of the superior orbital fissure. Neurosurgery 36:762-775, 1995
- Ohmoto T, Nagao S, Mino S, et al: Exposure of the intracavernous carotid artery in aneurysm surgery. Neurosurgery 28:317-324, 1991
- Parkinson D: A surgical approach to the cavernous portion of the carotid artery. Anatomical studies and case report. J Neurosurg 23:474-483, 1965
- Parkinson D: Surgical anatomy of the lateral sellar compartment (cavernous sinus). Clin Neurosurg 36:219-239, 1990
- Paullus WS, Pait TG, Rhoton AL, Jr. Microsurgical exposure of the petrous portion of the carotid artery. J Neurosurg 47:713-726, 1977
- Perneczky A, Knosp E, Matula C: Cavernous sinus surgery. Approach through the lateral wall. Acta Neurochir (Wien) 92:76-82, 1988
- Perneczky A, Knosp E, Vorkapic P, et al: Direct surgical approach to infraclinoidal aneurysms. Acta Neurochir (Wien) 76:36-44, 1985
- Renn WH, Rhoton AL, Jr. Microsurgical anatomy of the sellar region. J Neurosurg 43:288-298, 1975
- Rhoton AL, Jr., Hardy DG, Chambers SM: Microsurgical anatomy and dissection of the sphenoid bone, cavernous sinus and sellar region. Surg Neurol 12:63-104, 1979
- Rhoton AL, Jr., Inoue T: Microsurgical approach to the cavernous sinus. Clin Neurosurg 37:391-439, 1989
- Sadasivan B, Ma SH, Dujovny M, et al: The anterior cavernous sinus space. Acta Neurochir (Wien) 108:154-158, 1991
- Schnitzlein HN, Murtagh FR, Arrington JA, et al: The sinus of the dorsum sellae. Anat Rec 213:587-589, 1985
- Sekhar LN, Burgess J, Akin O: Anatomical study of the cavernous sinus emphasizing operative approaches and related vascular and neural reconstruction. Neurosurgery 21:806-816, 1987
- Sekhar LN, Schramm VL, Jr., Jones NF: Subtemporal-preauricular infratemporal fossa approach to large lateral and posterior cranial base neoplasms. J Neurosurg 67:488-499, 1987
- Sekhar LN, Sen CN: Comments on Inoue T, Rhotton AL, Jr., Theele, D, Barry ME: Surgical approaches to the cavernous sinus: A microsurgical study. Neurosurgery 26:932, 1990
- Spetzler RF, Fukushima T, Martin N, et al: Petrous carotid-to-intradural carotid saphenous vein graft for intracavernous giant aneurysm, tumor, and occlusive cerebrovascular disease. J Neurosurg 73:496-501, 1990
- Taptas JN: The so-called cavernous sinus: A review of the controversy and its implications for neurosurgeons. Neurosurgery 11:712-717, 1982
- Taptas JN: Must we still call cavernous sinus the parasellar vascular and nervous crossroads? The necessity of a definite topographical description of the region, in Dolenc VV (ed): The Cavernous Sinus. A Multidisciplinary Approach to Vascular
Tumorous Lesions. New York: Springer-Verlag, 1987, pp 30-40 - Umansky F, Nathan H: The lateral wall of the cavernous sinus. With special reference to the nerves related to it. J Neurosurg 56:228-234, 1982
- van Loveren HR, Keller JT, el-Kalliny M, et al: The Dolenc technique for cavernous sinus exploration (cadaveric prosection). Technical note. J Neurosurg 74:837-844, 1991
- van Overbeeke JJ, Dujovny M, Troost D: Anatomy of the sympathetic pathways in the cavernous sinus. Neurol Res 17:2-8, 1995
