
Frameless Stereotaxy and Minimally Invasive Neurosurgery: Case Report
Mark Gerber, MD
Kris A. Smith, MD
Division of Neurological Surgery, Barrow Neurological Institute, St. Joseph’s Hospital and Medical Center, Phoenix, Arizona
Abstract
Surgery for patients with refractory temporal lobe epilepsy has been affected favorably by frameless stereotaxy and minimally invasive surgery. Depth electrodes can be placed using a frameless stereotactic system, and a selective amygdalohippocampectomy for epilepsy caused by mesial temporal sclerosis can be performed through a minimally invasive approach. This case highlights such a surgical approach performed with frameless stereotaxy as an adjunct.
Key Words: epilepsy, frameless stereotaxy, minimally invasive surgery, selective amygdalohippocampectomy
The use of frameless stereotaxy as a surgical adjunct to a selective amygdalohippocampectomy is illustrated.
Illustrative Case
A 20-year-old male with complex partial seizures was evaluated by our epilepsy service. The patient reported having seizures since he was 16 years old. His seizures were preceded by a queasy feeling in his stomach and a chill and followed by chromatic aberrations in his visual fields. The patient’s current medications included carbamazepine and phenytoin, and he had been on divalproex and gaba pen tin in the past. Despite optimal medical management, he still had 30 to 90 simple partial seizures and 8 to 12 complex partial seizures per month.
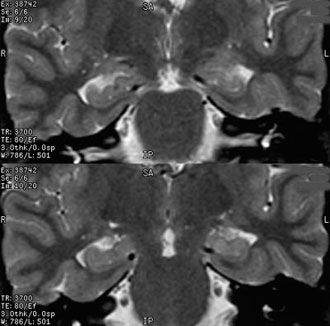
High-resolution magnetic resonance imaging of the brain demonstrated left mesial temporal sclerosis (Fig. 1). The patient was admitted to our Epilepsy Monitoring Unit for further evaluation. Electroencephalographic recording was consistent with a left temporal focus. The patient’s case was reviewed at the Multidisciplinary Epilepsy Conference, and a left selective amygdalohippocampectomy was recommended.
After informed consent for surgery was obtained, the patient was admitted to the hospital electively and underwent a left selective amygdalohippocampectomy. The surgery was performed using frameless stereotactic image guidance through a minimally invasive skin incision and craniotomy. The patient’s head was placed in a Mayfield headholder (Codman, Inc., Raynham, MA) and rotated toward the right, thereby exposing the left hemicranium. A small sandbag was placed under the patient’s left shoulder to facilitate rotation toward the left.
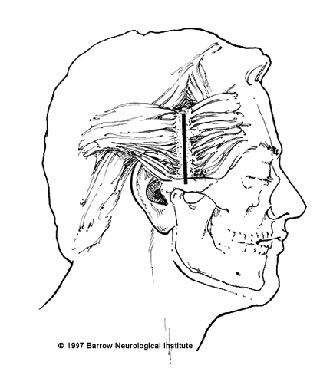
The frameless image-guidance system (ISG Wand, ISG Technologies, Mississauga, Ontario, Canada) was registered to the fiducials on the patient’s scalp. Using image guidance, a point on the skin in the preauricular area that overlaid the middle temporal sulcus was identified. A 5-cm linear skin incision, starting above the root of the zygoma and directed superiorly toward the superior temporal line (Fig. 2), was planned. The area was prepared and draped in the usual sterile fashion. The skin incision was made and the superior temporalis fascia identified. The temporalis fascia and muscle were divided and elevated. Fishhooks and a Greenberg retractor arm were configured to expose the temporal bone. At this point, the image-guidance system was again used to verify the location of the middle temporal sulcus.
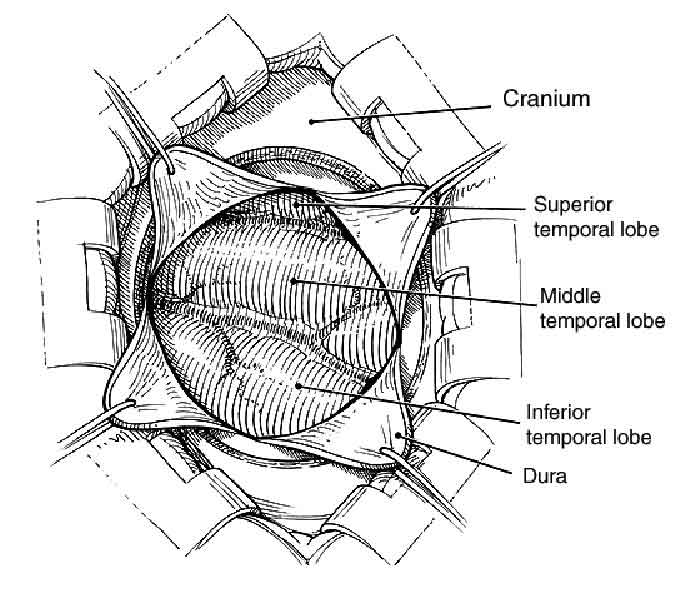
A 2.5-cm craniotomy was turned and elevated. The dura was opened in a cruciate fashion and tacked up with 4-0 Nurolon sutures (Ethicon, Johnson & Johnson Professionals, Inc., Somerville, NJ; Fig. 3). Using the operating microscope and image guidance, the middle temporal sulcus was opened and a corticectomy performed until the temporal horn of the left lateral ventricle was entered. Retractor blades were attached to the Greenberg arms to facilitate visualization into the lateral ventricle. Through this small opening, the hippocampus and amygdala were removed.
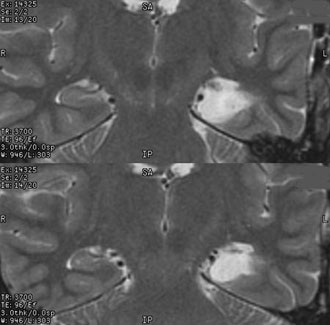
The patient spent the first postoperative night in the Intensive Care Unit. Postoperative imaging was obtained on Day 1 (Fig. 4), and the patient was discharged home on postoperative Day 2. Twenty-seven months after surgery, the patient’s seizures are under excellent control. He has retained a valid driver’s license and also has gotten married.
Discussion
Several studies have described the efficacy of selective amygdalohippo campectomy as a treatment for patients with mesial temporal sclerosis.[1] Frameless stereotaxy and image guidance have further enhanced the safety of this procedure by providing the ability to perform the surgery through a minimally invasive approach. Patients appear to tolerate the procedure well and tend to have a short, benign hospital course. A long-term follow-up of almost 70 patients indicates that the procedure is associated with favorable seizure control and no associated language or speech deficits (Smith K, unpublished data, 2001).
References
- Wieser HG, Yasargil MG: Selective amygdalohippocampectomy as a surgical treatment of mesiobasal limbic epilepsy. Surg Neurol 17:445-457, 1982
