
Arginine-Vasopressin Deficiency
Overview
Arginine-vasopressin deficiency (AVP-D) (formerly known as cranial or central diabetes insipidus) is a treatable condition affecting the body’s ability to regulate fluid balance. It can lead to excessive thirst and frequent, high-volume urination.
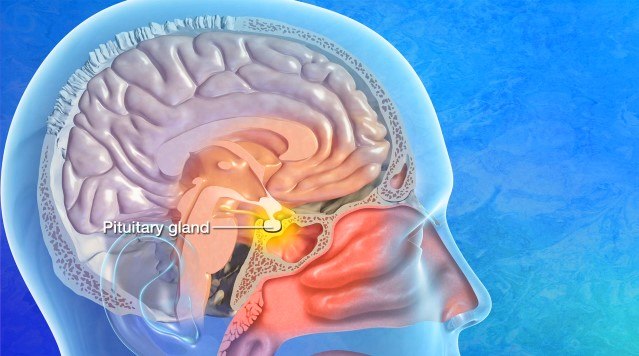
Normally, the hormone AVP regulates the body’s water balance by controlling the amount of water the kidneys reabsorb while filtering other body waste. In AVP-D, the hypothalamus isn’t making sufficient AVP, which results in the kidneys not being able to reabsorb water.
This condition was previously called diabetes insipidus, but this has caused some confusion and misunderstandings with diabetes mellitus, the type of diabetes that involves abnormal blood sugar control, resulting in high blood sugar. Therefore, the name diabetes insipidus was changed to AVP-D in 2024 to avoid this confusion. AVP-D can be mild or severe and chronic or temporary, depending on its cause.
What causes AVP-D?
Damage to the hypothalamus or pituitary gland is a common cause of AVP-D. This can be the result of a hypothalamic-pituitary tumor, treatment for these tumors with surgery, brain radiation, a head injury, autoimmune diseases, brain infections, or genetic disorders.

Arginine-Vasopressin Deficiency Symptoms
The main symptoms of AVP-D are excessive thirst and urination. Rarely, if the thirst center in the hypothalamus is damaged, you might lose the thirst sensation and not drink enough fluids to prevent dehydration, which can be dangerous.
If you or someone you know has AVP-D, you may experience the following:
- Excessive thirst: Also known as polydipsia, this condition causes an intense, constant urge to drink large amounts of fluids and a craving for cold water and ice.
- Frequent urination: Producing excessive amounts of light-colored, diluted, or clear urine each time you urinate, known as polyuria.
- Waking up at night: Frequent urination often disrupts sleep.
- Confusion or irritability: Imbalanced sodium levels can cause confusion or irritability.
- Dehydration: Dry skin and mouth, lightheadedness or dizziness, headaches, fatigue, rapid heart rate, and low blood pressure can develop if fluid loss isn’t balanced by drinking enough water.
- Muscle cramps or weakness: Dehydration and electrolyte shifts can trigger muscle cramps or unusual weakness.
- Nausea and vomiting: In severe cases of electrolyte imbalance, nausea and vomiting can occur.
If you’re experiencing uncontrollable thirst with excessive urination, symptoms of dehydration despite consuming fluids, or sudden changes in your mental state, like confusion or lethargy, please call 9-1-1. Severe dehydration is dangerous and can be life-threatening.
Diagnosis
AVP-D diagnosis typically involves a physical examination, urinalysis, blood tests, and occasionally a formal water deprivation test.
- Physical and neurological exam: First, your healthcare provider will ask about your symptoms, overall health, and family history. Next, they’ll complete an examination to assess neurological function, including reflexes, coordination, strength, and sensation.
- Urinalysis: This test will check your urine concentration to determine if it is too diluted and check your blood glucose level to rule out diabetes mellitus.
- Blood tests: A blood test will measure your blood concentration and sodium levels.
- Water deprivation test: If doctors can’t confirm your diagnosis with blood and urine tests, they may perform a water deprivation test. This test involves not drinking any liquid for several hours to monitor how your body responds. If you have AVP-D, you’ll continue to produce large amounts of diluted, light-colored urine rather than a small amount of concentrated, deep yellow urine. This test is done under medical supervision to ensure dehydration doesn’t occur.
- Magnetic resonance imaging (MRI): An MRI provides detailed images of the brain and its surrounding structures to detect tumors, trauma, or other structural abnormalities. In the event of AVP-D, an MRI will check for abnormalities of the pituitary gland or hypothalamus.
After your doctors use these tests to confirm your diagnosis, they can work with you to craft a treatment plan.
Arginine-Vasopressin Deficiency Treatment
Treatment focuses on managing symptoms, controlling urine output, preventing dehydration, and addressing the underlying cause.
Nonsurgical Treatments
For central diabetes insipidus (CDI), nonsurgical treatments can include:
- Desmopressin (DDAVP): As a synthetic form of AVP, desmopressin can be taken as a nasal spray, oral tablet, or injection to reduce urination and excessive thirst. Desmopressin mimics the actions of AVP and helps the kidneys retain water.
- Electrolyte monitoring and hydration management: Preventing sodium and electrolyte imbalances is vital, as excessive desmopressin can lead to excessive water retention, which in turn can lead to low sodium levels. Drinking enough water to prevent dehydration is also important.
- Behavioral therapy: Because adipsic AVP-D is caused by a defective thirst mechanism, partnering with a behavioral therapy professional to learn to control excessive or insufficient fluid intake can help. A plan to drink adequate fluids daily is also essential to prevent dehydration.
Common Questions
How common is AVP-D?
AVP-D affects around 1 in 25,000 people.
Who gets AVP-D?
Patients who have pituitary tumors affecting the hypothalamus and pituitary, surgery, brain radiation, head injury, autoimmune diseases, brain infections, or genetic disorders may get AVP-D.
What is the prognosis for those with AVP-D?
The prognosis of AVP-D depends on how well it’s managed. With appropriate treatment, most people can lead normal, healthy lives. For those with adipsic AVP-D, the prognosis varies by individual, but behavioral therapy and fluid intake control can help.
However, untreated AVP-D can lead to dehydration, electrolyte imbalances, and complications. The risk of these complications and death is higher for infants, seniors, and those with mental health conditions as they have difficulty recognizing their symptoms. An early diagnosis improves outcomes; it is crucial to contact your healthcare provider if you suspect AVP-D or are concerned about symptoms.
If AVP-D does develop, prompt medical intervention can help reduce the severity of the condition.



