Ischemic Stroke
Overview
Ischemic stroke occurs when a blockage causes inadequate blood flow to a part of the brain, depriving brain cells of vital oxygen and nutrients. This, in turn, leads to brain cell damage or death.
An estimated 1.9 million brain cells die during every minute of an ischemic stroke, making immediate medical treatment of stroke critical to save brain tissue and reduce long-term damage. In other words, “time is brain” when it comes to a stroke.
- Embolic stroke: This type of ischemic stroke occurs when a blood clot or other solids form elsewhere in the body—often the heart—and travels to the brain, blocking blood flow. Common contributing factors to an embolic stroke are atrial fibrillation, heart valve disease, or other cardiac conditions.
- Thrombotic stroke: This type of ischemic stroke happens when a blood clot forms in one of the arteries supplying blood to the brain or inside an artery within the brain. A thrombotic stroke is often due to atherosclerosis, or plaque buildup that leads to the narrowing of arteries.
- Lacunar stroke: Also known as small vessel disease, this is an ischemic stroke caused by a blockage in one of the small arteries deep within the brain. Chronic high blood pressure or diabetes, which damages small blood vessels over time, are typical causes.
- Watershed stroke: This type of ischemic stroke takes place in the “border zones” between major cerebral arteries and is caused by low blood flow as a result of severe hypotension—known as low blood pressure—or cardiac arrest.
- Cryptogenic stroke: This type of stroke has no clear or definite cause and is only identified when other causes, like atherosclerosis, small-vessel disease, or heart embolisms, are ruled out. Most cryptogenic strokes result from a blockage in blood flow to the brain, meaning they meet the definition of an ischemic stroke.
- Transient ischemic attack (TIA): Also known as a “mini stroke,” a TIA is a disturbance in brain function caused by a temporary blockage of blood to the brain that resolves. While there’s usually no permanent injury to the brain, it’s a warning sign that a major stroke may happen soon.
When to call 9-1-1: Any kind of ischemic stroke can be life-threatening and warrants immediate medical attention.
If you or someone around you experience sudden balance or vision problems, confusion or cognitive issues, dizziness or loss of coordination, seizures, or incontinence, call 9-1-1 and wait for help to arrive.
What causes an ischemic stroke?
The most common risk factor in ischemic stroke is high blood pressure, known as hypertension. Other leading causes include:
- Atherosclerosis
- Blood clots
- Heart conditions like atrial fibrillation or irregular heartbeat
- Heart valve disease
- Blood disorders like sickle cell disease, inflammation of blood vessels, or even severe dehydration can also increase the risk of stroke.
There’s also a high risk of hemorrhagic stroke following an ischemic stroke. Called a hemorrhagic conversion, the risk of hemorrhagic stroke increases dramatically in the days (up to two weeks) after a large ischemic stroke.
In addition to these causes, modifiable and non-modifiable risk factors can increase your likelihood of a stroke. Modifiable risk factors, or risk factors that you can influence or change, include:
- Uncontrolled high blood pressure
- Diabetes
- High cholesterol
- Smoking
- Excessive alcohol use
- Poor diet, particularly one high in salt, sugar, and saturated fats
- Obesity and a sedentary lifestyle
Factors that you cannot influence or change, called non-modifiable risk factors, include:
- Your age and gender: The risk of stroke increases with age, and women are at a slightly higher lifetime risk of stroke than men.
- Your genetic predispositions: A family history of stroke or vascular disease affects overall stroke likelihood.
- Your race: People of African American or Hispanic descent have a higher stroke risk, partially due to higher rates of hypertension and diabetes.
Regular check-ups with your healthcare team can help you recognize and manage these risk factors and significantly reduce stroke risk.

Ischemic Stroke Symptoms
The signs of a stroke depend on which side of your brain is affected, the structure or structures of the brain affected, and the severity of the stroke. This means that each person may experience different warning signs.
The most common symptom of ischemic stroke is a sudden weakness of the face, arm, or leg, usually on one side of the body. Someone having an ischemic stroke may experience the following symptoms:
- Sudden changes like confusion, difficulty speaking, or difficulty understanding speech
- Vision problems, such as double vision or blindness in one or both eyes
- Impaired consciousness or confusion
- Dizziness and vertigo
- Loss of coordination
- Seizure
- Urinary incontinence
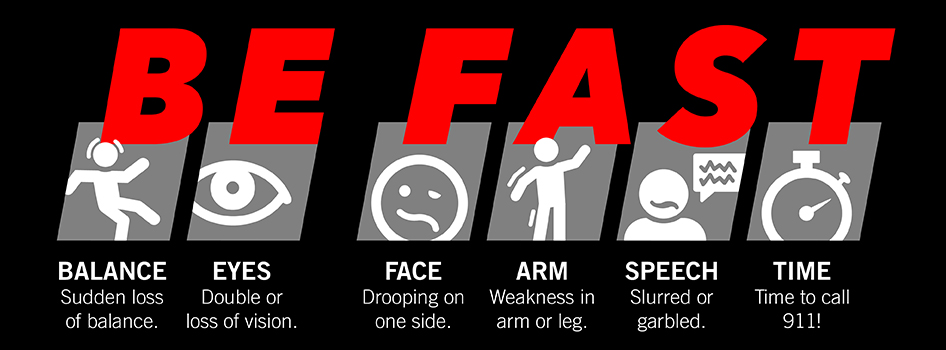
Recognizing a stroke quickly and calling 9-1-1 leads to faster diagnosis, treatment, and better recovery. People should “BE FAST” when it comes to stroke.
Here’s how to BE FAST:
- B – BALANCE: Ask the person to walk. Do they have trouble keeping their balance or walking normally?
- E – EYES: Ask the person about their eyesight. Have they lost vision or experienced vision changes in one or both eyes?
- F – FACE: Ask the person to smile. Does one side of the face droop?
- A – ARMS: Ask the person to raise both arms. Does one arm drift downward?
- S – SPEECH: Ask the person to repeat a simple phrase. Is their speech slurred or strange?
- T – TIME: If you observe any of these signs, call 9-1-1 immediately.
Ischemic Stroke Diagnosis
Diagnosing an ischemic stroke is a critical and time-sensitive process, as early detection can vastly improve treatment outcomes. Brain imaging should be done immediately upon hospital arrival or curbside in a mobile stroke unit to confirm the diagnosis. Ideally, diagnosis happens within 60 minutes or less from when the symptoms are first noticed.
If you have the symptoms of an ischemic stroke or a transient ischemic attack (TIA), your care team will perform several of the following tests and exams to reach a diagnosis quickly:
- Physical and neurological exam: Your healthcare provider will ask about your symptoms, overall health, and family history of stroke or related conditions. Next, they’ll complete a neurological examination to assess your neurological function, including reflexes, coordination, strength, and sensation.
- Imaging tests: Either magnetic resonance imaging (MRI) or a computed tomography (CT) scan will allow doctors to differentiate between an ischemic stroke and a hemorrhagic stroke and treat it appropriately. While MRI is more sensitive to subtle changes in cerebral blood flow, CT is generally performed first because it can be performed rapidly in a wider variety of settings (for example, in a mobile stroke unit).
- Electrocardiogram (ECG): An electrocardiogram is a simple and timely test that records electrical signals in the heart and can detect irregular heart rhythms.
- Echocardiogram: Also known as an “echo,” an echocardiogram is a non-invasive imaging test that uses ultrasound waves to create detailed pictures of the heart and its structure, function, and movement.
- Cerebrovascular testing: This group of testing describes the various tools used to diagnose conditions affecting the blood vessels inside and around the brain.
- CT angiography (CTA) or magnetic resonance angiography (MRA): CT angiography uses dye and a CT scan to visualize blood vessels to detect blockages, narrowing, or clots in the arteries, while magnetic resonance angiography relies on MRI technology.
- Blood tests: These include a complete blood count (CBC) to check for infection, clotting issues, or anemia; coagulation tests to assess blood clotting ability; glucose levels to rule out hypoglycemia; lipid panels to check cholesterol; and markers for infectious or clotting disorders.
Ideally, an initial assessment is completed within 10 minutes. Within 25 minutes, an MRI or CT scan is done. And in 60 minutes or less, a diagnosis is made and treatment is initiated.
Our team at Barrow Neurological Institute’s Petznick Stroke Center can perform a full range of diagnostic tests to determine the exact cause of a stroke 24 hours a day, seven days a week.

Ischemic Stroke Treatment
Doctors can minimize the impact of an ischemic stroke by initiating treatment within the first four hours and 30 minutes of symptoms starting. The longer a stroke goes untreated, the more brain cells die, and the more difficult recovery becomes.
As a whole, ischemic stroke treatments focus on restoring blood flow to the brain, stemming additional damage, and reducing the risk of future strokes.
Nonsurgical Treatments
- Thrombolytic therapy: For the first 4.5 hours after a stroke, IV administration of a “clot-busting” medication called tenecteplase (TNK) can dissolve the blood clot and restore crucial blood flow to the brain. However, to be effective, doctors must give this treatment within 4.5 hours of the last time a person was known to be well. This is because TNK doesn’t improve outcomes after the first 4.5 hours of symptoms appearing.
- Antiplatelet therapy: Doctors can administer medications like aspirin, clopidogrel (Plavix), or dipyridamole to prevent platelets from clumping together and forming new clots, reducing the risk of additional strokes.
- Anticoagulant therapy: Blood thinners like warfarin or direct oral anticoagulants (DOACs) prevent new clots from forming or existing clots from growing and may be prescribed for conditions like atrial fibrillation.
- Blood pressure management: Since high blood pressure is the most common risk factor for stroke, medications to lower or stabilize blood pressure are often an essential part of treatment.
- Cholesterol-lowering drugs: Drugs like statins play a crucial role in managing stroke risk by lowering cholesterol levels and improving outcomes after a stroke.
- Anti-seizure medications: If a stroke causes seizures or there’s a high risk of them occurring, your doctor will prescribe anti-seizure medications will be prescribed.
- Blood sugar control: Maintaining optimal blood glucose levels with insulin or oral medications reduces the risk of stroke complications and further damage for those with diabetes.

Barrow Mobile Stroke Unit
The Barrow Mobile Stroke Unit has a CT scanner, stroke-specific medications, and a specially trained team, including a nurse, paramedic, CT tech, and a neurologist who can join remotely by video. This allows them to scan the patient’s brain on the spot to see if a blocked blood vessel or bleeding causes the stroke. If an ischemic stroke is confirmed, the team can administer TNK immediately, saving precious time.
As a whole, ischemic stroke treatments focus on restoring blood flow to the brain, stemming additional damage, and reducing the risk of future strokes.
Surgical Treatments
- Thrombectomy: Doctors may use this minimally invasive surgical procedure when a large artery blockage causes a stroke. In this procedure, a surgeon mechanically removes the blood clot by breaking it up and removing the pieces through a catheter or retrieving it with a stent device. However, this treatment must be done within 24 hours of the onset of symptoms.
- Carotid endarterectomy: This surgical procedure removes plaque buildup from the carotid arteries, or large blood vessels in the neck that supply blood to the brain, face, and head. It also helps to reduce the risk of future strokes.
- Angioplasty: This is a minimally invasive medical procedure used to open narrowed or blocked blood vessels and restore proper blood flow. In this procedure, a balloon is used to widen the narrowed arteries, and if needed, a stent—or small, wire mesh tube—is placed to keep them open.
One Central Location with Multiple Treatment Options
At the Petznick Stroke Center at Barrow Neurological Institute, we’re dedicated to best-in-class stroke care and exhaustive research to find new ways to treat and prevent stroke. Our Center cares for more stroke victims than any other center in the southwestern U.S. We’re also a leading stroke research center, conducting more clinical and prevention trials than any other institution in the region.
From curbside care in our mobile stroke unit to reintegration into the community after a stroke, our Petznick Stroke Center offers a complete spectrum of care for you or your loved one.
Neuro-Rehabilitation for Quality of Life
Neuro-rehabilitation is key to stroke recovery. While it doesn’t reverse brain damage, neuro-rehabilitation can help stroke patients achieve the best long-term outcome possible.
You or your loved one’s rehabilitation treatments will vary, depending on the part of the brain that’s been affected and the severity of the stroke. Treatments will be provided in an acute care hospital, a rehabilitation inpatient hospital, or an outpatient setting. At Barrow Neurological Institute, our CARF-accredited Neuro-Rehabilitation Center offers inpatient, outpatient, and transitional rehabilitation programs. We also lead the industry in using neuro-robotics. These cutting-edge technologies allow patients to reach unprecedented heights in function and independence.
Lastly, it’s important to remember that after a stroke, depression and anxiety have a greater likelihood of developing: about one in three people in the first year develop depression, while one in four develop anxiety. While it’s easy to focus solely on the physical recovery, your emotional health is equally important. Please get in touch with your healthcare provider if you suspect you or someone you love may be struggling with either condition.
Common Questions
How common is an ischemic stroke?
Nearly 800,000 people experience a stroke each year. Of this number, 690,000 of them are ischemic strokes—87 percent of all strokes, according to the American Stroke Association.
Who is likely to experience an ischemic stroke?
Ischemic stroke can happen at any age, but stroke risk doubles for each decade after age 55. Men are slightly more likely to have a stroke at younger ages. At the same time, women face higher stroke risk overall due to their longer life expectancy.
While men are more likely to have an ischemic stroke than women, women are more likely to suffer a fatal stroke. Pregnancy and the use of birth control pills can pose a unique risk for women, although the stroke risk from combined oral contraceptives is lower than the risk of stroke during pregnancy.
The risk of having a stroke is nearly twice as high for black people as it is for white people. Stroke incidence is also higher for Hispanic people compared to non-Hispanic people, with an increasing trend of stroke risk in younger individuals.
Additionally, if you’ve had a stroke, you’re at high risk for experiencing another one: one in four stroke survivors has had another stroke within five years of the first one.
Other risk factors include high blood pressure, high cholesterol, heart disease, diabetes, and sickle cell disease.
What is the prognosis for someone who experiences an ischemic stroke?
The prognosis for someone who’s had a stroke depends on multiple factors, including the type of stroke, its severity, the area of the brain affected, how quickly treatment was received, and the person’s overall health. Some individuals recover fully, while others may experience long-term or permanent disabilities.
In ischemic strokes, the prognosis tends to be better than in hemorrhagic strokes. Early treatment with clot-busting drugs or thrombectomy therapy significantly improves outcomes.
Some individuals regain all pre-stroke abilities, especially following mild strokes or those with timely treatment. Many stroke survivors experience a partial recovery, meaning they can have lasting impairments, like weakness or paralysis on one side, difficulty with balance, coordination, or swallowing, or residual speech and language problems. In some cases, strokes result in severe disability, such as memory loss or reduced executive function and dependence on caregivers for daily activities.
As a whole, faster treatment for all strokes leads to better outcomes. So, too, does the effective management of modifiable risk factors, like high blood pressure or obesity.
Can an ischemic stroke be prevented?
The good news is that most strokes are preventable. Approximately 80 percent of all strokes can be prevented by lifestyle and behavior modification and control of healthcare conditions like diabetes, obesity, and high cholesterol.
If you have any of the following risk factors, please speak with your trusted healthcare professional to come up with a plan to reduce your stroke risk:
- High blood pressure, specifically systolic blood pressure greater than 140 mm/Hg and diastolic blood pressure greater than 85 mm/HG
- Smoking
- Excessive alcohol consumption
- Physical inactivity and obesity
- Diabetes, specifically Hemoglobin A1c above 5.7 percent
- Hypercholesterolemia, or high levels of “bad cholesterol” (LDL)
Resources
American Stroke Association: Ischemic Stroke
National Institute of Neurological Disorders and Stroke (NINDS)