Anti MOG Syndrome
Overview
Anti-MOG syndrome is an autoimmune disorder in which the immune system mistakenly attacks myelin oligodendrocyte glycoprotein (MOG). This protein is located on the surface of myelin, an insulating layer that protects nerve cells and helps facilitate communication between them. When the immune system attacks MOG, it produces antibodies to the protein.
Antibodies normally protect us from viruses and bacteria, but antibodies to MOG can cause the myelin sheath to fall off nerve cells. This process, known as demyelination, can prevent the neurons from transmitting messages effectively and result in neurological symptoms.
Symptoms of anti-MOG syndrome
Individuals with anti-MOG syndrome may experience optic neuritis, transverse myelitis, and/or acute dissemination encephalomyelitis, depending on which parts of their nervous system are affected.
Symptoms of acute disseminated encephalomyelitis may include:
- Coma
- Confusion
- Drowsiness
- Fever
- Headache
- Numbness or tingling (sensory changes)
- Seizures
- Trouble swallowing
- Unsteady walk (ataxia)
- Weakness in arms or leg
Symptoms of optic neuritis may include:
- Blurry or otherwise disturbed vision
- Color blindness
- Eye pain that worsens with eye movement
- Vision loss or severely impaired vision in one eye
Symptoms of transverse myelitis, which tend to develop rapidly over several hours to several weeks, may include:
- Back pain
- Bowel and bladder dysfunction
- Feeling that something is wrapped around your stomach and lower back
- Limb weakness or paralysis, beginning in your legs and moving up your body
- Sensory disturbances, such as numbness or sensitivity to touch

Treatment
Treatment for acute symptoms of demyelination involves reducing inflammation. Intravenous corticosteroids are the first line of treatment. In rare cases, if high-dose steroids are not effective, patients may undergo intravenous immunoglobulin (IVIG) treatment.
Many individuals with anti-MOG syndrome will recover fully after their first treatment and never relapse. However, some patients may experience recurrent attacks and need a long-term management plan. This may include IVIG and medication, such as azathioprine, myucophenolate mofetil, or rituximab.
Common Questions
How common is anti-MOG syndrome?
Anti-MOG syndrome is rare. A 2019 study reported the incidence of anti-MOG syndrome as 1.6 per 1 million people.
Who gets anti-MOG syndrome?
Anti-MOG syndrome affects men and women equally, and disease onset usually occurs in a person’s 20s or 30s. Research suggests that people who are white may be affected more frequently than people of other races.
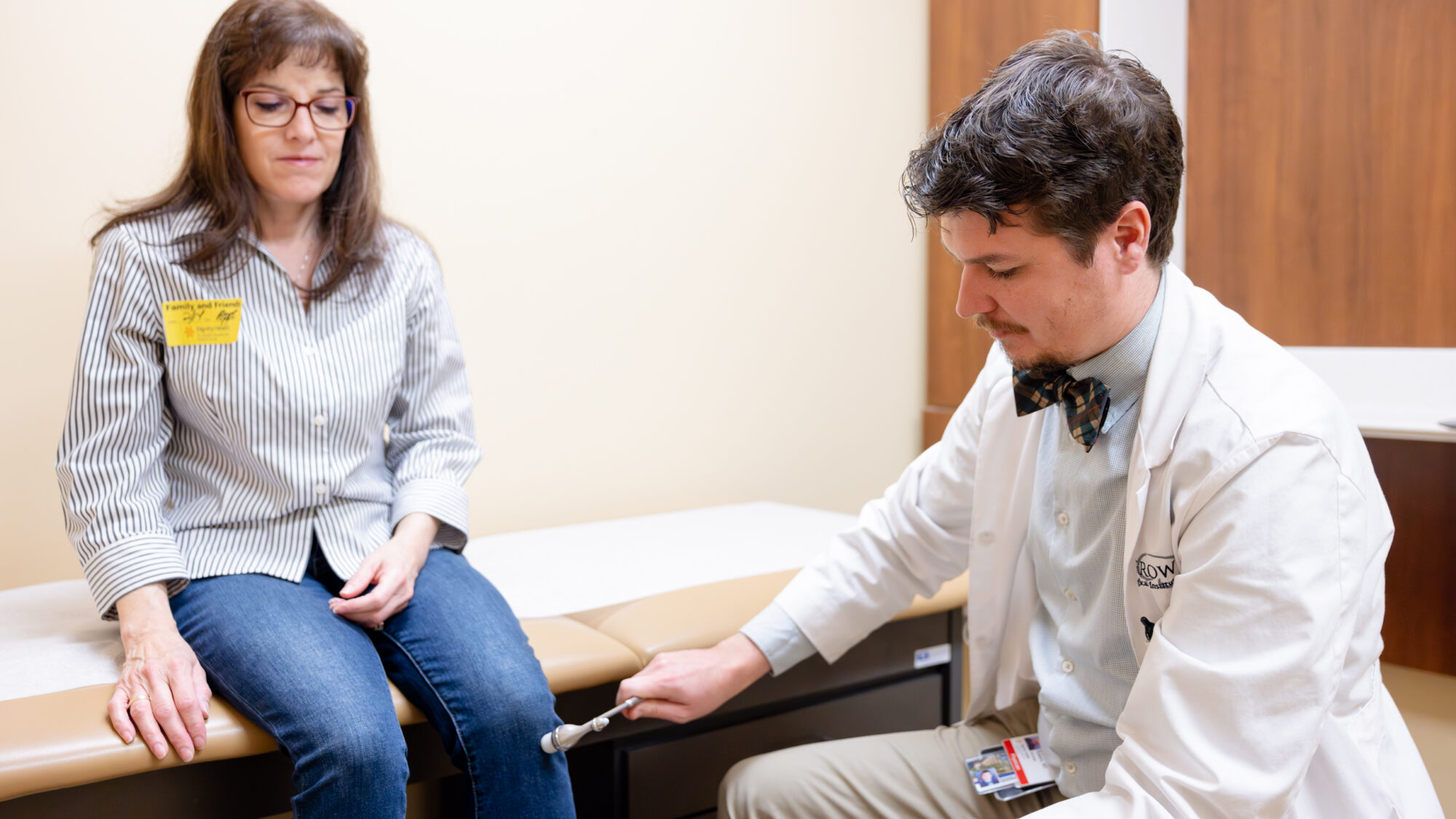
How is anti-MOG syndrome diagnosed?
Your doctor will look for symptoms of neuroinflammatory diseases that may occur with anti-MOG syndrome, such as optic neuritis, transverse myelitis, and acute disseminated encephalomyelitis.
The following tests can help confirm anti-MOG syndrome:
- Blood tests to check for MOG antibodies
- Eye assessment to evaluate optic nerve for inflammation
- Lumbar puncture to evaluate cerebrospinal fluid (CSF)
- Magnetic resonance imaging (MRI) to see where inflammation has occurred



