
Familial Isolated Pituitary Adenoma (FIPA)
Overview
Familial isolated pituitary adenoma (FIPA) is a condition that leads to the development of pituitary tumors within families.
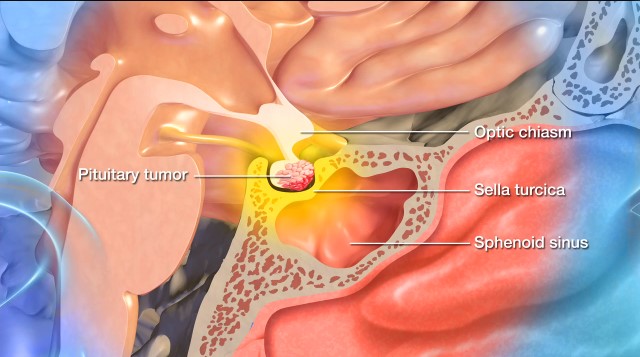
A pituitary tumor—also commonly referred to as a pituitary adenoma—is an abnormal growth of cells within or around the pituitary gland, a pea-sized organ at the base of the brain. These benign tumors can lead to hormone imbalances or other health issues. However, FIPA will not increase the risk of tumors growing elsewhere in the body.
A diagnosis of FIPA requires that two or more family members develop pituitary adenomas without signs of another syndrome that causes these tumors. Families diagnosed with FIPA are fortunately rare, making up approximately two to five percent of all pituitary tumors.
What causes familial isolated pituitary adenomas?
The following inherited genetic mutations cause familial isolated pituitary tumors (FIPA):
- AIP Gene Mutations: The aryl hydrocarbon receptor-interacting protein—also known as the AIP gene—occurs in 15 to 25 percent of FIPA families. These mutations are inherited in an autosomal dominant pattern, meaning a parent with the mutation has a 50 percent chance of passing it on to their child. AIP gene mutations are especially linked to growth hormone (GH)-secreting tumors, which can cause gigantism or acromegaly. Approximately 1 in 5 people with an AIP gene mutation will develop a pituitary tumor in their lifetime.
- Other Genetic Factors: In many cases, no known mutation is found, meaning the cause of the condition is a mutation-negative FIPA. In these instances, the theory is that undiscovered genes play a role.
It’s important to point out that doctors only diagnose FIPA when pituitary tumors run in families without other endocrine tumors, such as multiple endocrine neoplasia type 1 (MEN1). This means that a FIPA diagnosis is excluded if you or a family member has a history of MEN1 endocrine tumors.

Familial Isolated Pituitary Adenoma (FIPA) Symptoms
The symptoms of familial isolated pituitary adenoma (FIPA) tend to be the same as those of pituitary tumors. However, FIPA has a few key distinctions: the tumors often appear at a younger age, tend to be larger and grow more aggressively, and are diagnosed in two or more members of an immediate family.
Symptoms from a pituitary tumor are often the result of hormonal imbalances caused by the tumor, or from the tumor putting pressure on the pituitary gland or nearby structures. If you or someone you know has a pituitary tumor due to FIPA, you might experience a combination of the following symptoms:
Symptoms caused by pituitary tumor hormonal imbalances:
- Fatigue: Pituitary tumors can cause hormone reduction and overproduction, and this lack of hormones for energy regulation can lead to fatigue.
- Menstrual or Breast Changes: While these symptoms are often subtle, menstrual irregularities or cessation in your menstrual cycle can be indicative of a tumor that secretes high levels of prolactin.
- Change to Libido: Decreased sexual drive, as well as erectile dysfunction, can be caused by pituitary tumors, including FIPA.
- Unexplained Weight Gain: A sudden or unexpected weight gain, particularly in the face, upper back, and abdomen, can occur.
- Mood Changes: Pituitary tumors can cause mood changes, like depression, anxiety, or irritability, due to their effects on hormone levels and brain function.
- Unexplained Sleep Disruption: Hormonal imbalances, particularly cortisol-related imbalances, can disrupt the sleep-wake cycle.
- Unexplained Hair Growth or Loss: Lowered or heightened levels of certain hormones can cause hair growth or loss.
- Joint Pain and Skin Changes: A host of symptoms, like thickening skin, joint pain, enlarged hands, feet, and facial features, can occur. In adults, this is known as acromegaly, while in children, it’s called gigantism.
- Dizziness: Hormonal imbalances and secondary effects on blood pressure can lead to dizziness.
Symptoms caused by pituitary tumor pressure:
- Headaches: A prevalent symptom, headaches result from the tumor compressing pituitary tissue, which then leads to changes in intracranial pressure. Pituitary tumor headaches are typically located on the forehead or behind the eyes, but can vary in location and intensity.
- Vision Problems: Pituitary tumors can pressure the optic nerve, causing vision problems, especially loss of peripheral vision and double vision. In advanced cases, progressive vision loss or blindness can occur.
- Nausea and Vomiting: Increased intracranial pressure can also irritate the brain’s vomiting center, leading to nausea and vomiting.
- Dizziness: Pressure on nearby brain structures and secondary effects on blood pressure can lead to dizziness.
Symptoms like a severe headache, dramatic changes to your vision, and sudden hormonal changes should prompt an immediate medical evaluation. These can be symptoms of pituitary apoplexy, or sudden tumor bleeding.
Doctors recommend genetic counseling and testing for patients with a family history of pituitary tumors, as early detection and treatment can prevent complications and improve outcomes.
Familial Isolated Pituitary Adenoma (FIPA) Diagnosis
Familial isolated pituitary adenoma (FIPA) diagnosis requires the identification of pituitary tumors in two or more related family members through a combination of evaluation, imaging, and testing.
Doctors commonly use the following exams and tests in diagnosing FIPA:
- Physical and Neurological Exam: First, your healthcare provider will ask about your symptoms, overall health, and family history. Next, they’ll complete an examination to assess your neurological function, including reflexes, coordination, strength, and sensation.
- Magnetic Resonance Imaging (MRI): Imaging studies are crucial in visualizing the brain and identifying abnormalities, and an MRI is a gold standard for pituitary tumors. An MRI will provide detailed images of the pituitary gland and its surrounding structures and can detect the size and location of the tumor.
- Hormonal Testing: When it comes to pituitary tumors, specific tests are needed to assess your pituitary function and measure the levels of hormones it produces. These tests can include blood and urine tests, as well as testing growth hormone levels, thyroid hormones, and prolactin.
- Genetic Testing: Genetic testing is recommended if you have a family history of pituitary tumors and are 30 years old or younger. In genetic testing, a blood sample is taken to extract DNA. Genetic counseling is usually recommended before AIP gene testing is performed.
You may also be referred to an eye doctor for a vision test since pituitary tumors can exert pressure on your optic nerves and cause vision problems.
A FIPA diagnosis is important because it allows for early screening of at-risk family members, especially children and adolescents, who may develop tumors at a younger age. It also helps tailor your treatment plan, especially if you have an aggressive tumor.
Familial Isolated Pituitary Adenoma (FIPA) Treatment
The frontline treatments for familial isolated pituitary adenoma (FIPA) are often the same as those for standard pituitary tumors. However, in FIPA—especially with AIP mutations—tumors usually appear earlier, grow more aggressively, and are harder to treat. Hence, management tends to be more proactive and intensive. Family history will also play a significant role in long-term monitoring and prevention strategies.
Nonsurgical Treatments
The following nonsurgical treatments for pituitary tumors can be used on their own or in conjunction with surgery:
- Medication: Several medications help manage pituitary tumors by lowering the amount of hormones the body makes or even shrinking certain types of tumors. If your hormones fall to unhealthy levels, your doctor may prescribe hormone replacement therapy to help them reach a healthy level again.
- Radiation Therapy: Doctors use radiation when the tumor continues to grow or secrete hormones despite medication, and surgery is not an option, or the surgery did not completely remove the tumor. Radiation therapy uses precisely aimed beams of radiation to destroy tumors in the body by damaging the DNA of tumor cells, which then lose their ability to reproduce and die. This treatment is non-invasive, with no recovery time required. However, its tumor-shrinking effects may take months or even years to develop.
- Radiosurgery: A form of radiation therapy, this treatment uses a radiation delivery system to focus on the site of the pituitary tumor and minimize the radiation dose to the brain. The two most common forms of radiosurgery are:
- Gamma Knife Radiosurgery: This technique destroys abnormal tissue using precise and focused radiation beams and is only lethal to cells within the immediate vicinity. It’s an outpatient procedure that doesn’t involve incisions and requires brief sedation under a general anesthetic.
- CyberKnife Radiosurgery: This technique uses targeted energy beams to destroy tumor tissue while sparing healthy tissue. It uses image-guided robotics to deliver surgically precise radiation to help destroy pituitary tumors. CyberKnife is also an outpatient procedure and does not require general anesthesia.
- Watchful Waiting: For pituitary tumors that don’t cause significant symptoms, regular monitoring instead of immediate treatment may be recommended. To adequately monitor tumor growth, periodic MRI scans and hormone testing will be done to look for changes. However, if your tumor is growing or starting to cause symptoms, surgical or nonsurgical interventions may become necessary.
Surgical Treatments
Doctors might suggest surgery when pituitary tumors cause hormonal imbalances, put pressure on nearby structures, or do not respond to medication. The type of surgical approach will depend on the tumor’s size, type, location, and impact on surrounding tissues.
- Transsphenoidal Surgery: The most common surgical approach for a pituitary tumor is transsphenoidal surgery. This is when a neurosurgeon reaches and removes the tumor through the nasal passages and the sphenoid sinus using a small surgical instrument and an endoscope. Transsphenoidal surgery works best on small to medium-sized pituitary tumors confined to the sella turcica—the bony compartment of the pituitary gland—and leaves no scar. It also minimizes the risk of complications and offers a faster recovery.
- Craniotomy: Rarely, larger and more complicated pituitary tumors may require the surgical opening of your skull, known as a craniotomy. During a craniotomy, a neurosurgeon will make an incision in the scalp, remove a portion of the skull, and access the brain to remove the tumor, all while using intraoperative imaging and highly specialized tools to visualize and safely remove the tumor. This procedure is more invasive than transsphenoidal surgery and requires a longer recovery time.
One Central Location with Multiple Treatment Options
At Barrow Neurological Institute’s renowned Pituitary Center, we treat people with all forms of pituitary tumors and disorders in one dedicated location. And because our doctors and nurses treat more people with pituitary disorders than any other team in the Southwestern United States, you can rest assured you’ll be in experienced hands.
Common Questions
How common is familial isolated pituitary adenoma?
Familial isolated pituitary adenoma (FIPA) is a rare genetic condition, but it’s the most common hereditary form of pituitary tumors and accounts for around two to five percent of all pituitary tumor cases. Because many pituitary tumors are small and asymptomatic, and genetic testing isn’t routine for all cases, the actual number of FIPA cases may be underestimated.
While most pituitary tumors are sporadic—meaning they’re not inherited—about 1 in 20 pituitary tumors are linked to a family history, and many of those tumors will fall under the FIPA classification.
Who gets familial isolated pituitary adenoma?
Anyone with a family history of pituitary tumors is at risk. However, the type of pituitary tumor that develops can differ among family members. For example, one person may develop a prolactinoma, while another has a GH-secreting adenoma.
FIPA often appears in teens or young adults, especially in families with AIP mutations. Both men and women can be affected, though some studies suggest AIP-mutated FIPA may be slightly more common or more severe in males.
What is the prognosis for someone with familial isolated pituitary adenoma?
The prognosis for someone diagnosed with familial isolated pituitary adenoma (FIPA) will depend on the following features/elements:
- Type of pituitary tumor
- Size and invasiveness of the tumor
- Specific genetic mutations involved
- Age at diagnosis
- Response to treatment
However, with early detection and proper management, many individuals with FIPA will lead normal lives. Those with AIP mutations—the most common gene mutation—will often benefit from more aggressive early intervention. In the long term, ongoing monitoring via magnetic resonance imaging (MRI) and hormone testing is required.
Can familial isolated pituitary adenoma be prevented?
There isn’t anything you can do to prevent familial isolated pituitary adenoma (FIPA) since it’s an inherited genetic condition. However, the following steps can help manage your risk and improve outcomes:
- Genetic testing and counseling: If doctors have diagnosed FIPA in your family, genetic testing can help identify other at-risk family members. Meanwhile, genetic counseling will help each family member understand their risk and available options.
- Screening and early detection: For those with a family history of FIPA or an identified AIP mutation, routine screenings as early as childhood can detect the tumors early, even before symptoms develop.
- Monitoring: Even when someone with a family history of FIPA doesn’t initially show signs, regular monitoring can continue to help catch any changes early on.



