
Radiation-Induced Intracranial Malignant Fibrous Histiocytoma with a 37-Year Latency: Case Report
Authors
Bruce D. Jones, BA*
Michael T. Lawton, MD†
Martin C. Holland, MD†
Robert F. Spetzler, MD†
*Chicago College of Osteopathic Medicine, Chicago, Illinois
†Division of Neurological Surgery, Barrow Neurological Institute, St. Joseph’s Hospital and Medical Center, Phoenix, Arizona
Key Words : histiocytoma, radiation, retinoblastoma, transfacial approach
Malignant fibrous histiocytoma is a pleomorphic tumor of adults that usually occurs in the soft tissues of the extremities but that can also occur intracranially.3 Intracranial malignant fibrous histiocytoma has been observed in patients after radiation therapy for pituitary adenoma, rhabdomyosarcoma, retinoblastoma, and other conditions.8,9 In these cases, the latency from the time of irradiation to the occurrence of the malignant fibrous histiocytoma has ranged from 1.5 to 19 years.6-13,15 We describe a case of intracranial malignant fibrous histiocytoma that arose 37 years after the patient’s radiation treatment. This case represents the longest reported latency for intracranial malignant fibrous histiocytoma in the literature.
Case Studies
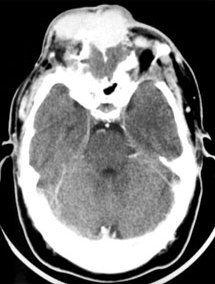
A 39-year-old Caucasian male presented with a painful frontal mass (Fig. 1). He had been born with bilateral retinoblastoma and had undergone enucleation of the left eye plus radiation treatment to the right eye. He was well until the age of 37 years when he developed a small mass in the radiation field. The mass was over his left eye and extended posteriorly into both frontal sinuses. It had been resected by an otolaryngologist, who initially diagnosed the lesion as a mucocele. Pathological analysis revealed a malignant fibrous histiocytoma. Postoperatively, the patient underwent two rounds of chemotherapy with adriamycin/ dacarbazine and ifosfamide/etoposide. Eighteen months later the mass on his forehead recurred and en-larged progressively during the next 6 months.
When the patient presented to our institution, the mass had occluded his right eye completely. His forehead was deformed by the large lobulated mass, which was tender to palpation. There was neovascularity of the overlying skin. Neurologically, he had limited upward movement of his right eye, which was compressed by the tumor. Vision in the right eye was present but acuity was decreased markedly (20/400). The remainder of his neurological examination was normal.
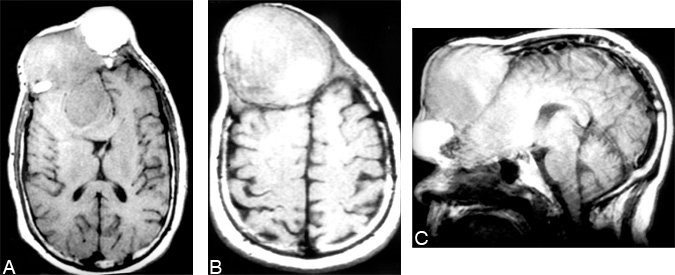
Magnetic resonance (MR) imaging showed a 9 x 9 x 9 heterogenous extra-axial mass in the right frontal region that had eroded the frontal bone (Fig. 2). The mass extended posteriorly to compress the right frontal lobe. The adjacent brain was edematous, and the frontal horn of the right lateral ventricle was effaced with a right-to-left midline shift. Cerebral angiography demonstrated bilateral vascular supply from the superficial temporal and middle meningeal arteries as well as from the left ophthalmic artery.
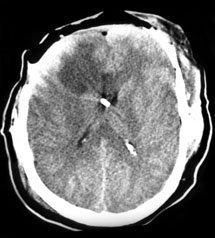
The patient underwent a transfacial approach with a bifrontal craniotomy and level one orbital osteotomy.2,10 The tumor had invaded the frontal bone, cribriform plate, and orbital roofs bilaterally and had penetrated dura to involve the subdural space. The tumor, involved bone, and involved dura were excised along with the anterior third of falx (Fig. 3). Adjacent brain was decompressed and the dural defect was repaired with a fascia lata graft. The anterior cranial floor was reconstructed with split-thickness cranial grafts and temporalis muscle flaps.
The tumor specimen was tan and marbled with green and gray tissue. The mass was encapsulated with central areas of necrosis. Microscopically, marked pleomorphism, multinucleated giant cells, and cartwheel formations were noted, consistent with the diagnosis of malignant fibrous histiocytoma.
The patient’s postoperative course was uneventful. The tumor, however, recurred 3 months after his discharge and he underwent a second resection. I125 seeds (40 seeds at 0.4 mCi/seed) were implanted in the resection bed. Two months later the patient was found to have lung metastases and he died 6 months thereafter.
Discussion
Malignant fibrous histiocytoma is a soft tissue tumor characterized histologically by a mixture of fibroblastic type cells and histiocytic cells arranged in a storiform growth pattern. In one large series,4 radiation was the cause of this tumor in 5% of the patients. The mean latency for malignant fibrous histiocytoma to develop after radiation therapy is 10 years and appears to be inversely proportional to the radiation dose.4,11 Primary intracranial malignant fibrous histiocytoma is rare. In 1976 Gonzalez-Vitale and coworkers8 reported the first such case, which occurred 11 years after radiation therapy for a pituitary adenoma. The longest previously reported latency for an intracranial malignant fibrous histiocytoma was 19 years after radiation for bilateral retinoblastoma.13 The 37-year latency in our patient represents a dramatically longer latency period for intracranial malignant fibrous histiocytoma than has previously been reported.
This case demonstrates that malignant fibrous histiocytoma can arise more than 30 years after radiation treatment. Consequently, patients treated with radiation should be followed throughout their lives. Bilateral retinoblastoma carries an increased risk of secondary tumors, which is further increased by radiation therapy. Roarty and coworkers14 reported a 30-year incidence of 5.8% in nonirradiated patients with bilateral retinoblastoma compared to a 30-year incidence of 35.1% in irradiated patients. However, none of the tumors in their series were reported to be malignant fibrous histiocytoma. Abramson and colleagues1reported a significantly higher incidence of secondary tumors—as high as 90% at 30 years—and 2 of 89 tumors were malignant fibrous histiocytomas. Neither of these studies followed patients more than 30 years after radiation therapy.
Prognosis for patients with radiation-induced malignant fibrous histiocytoma is poor, with a 5-year survival rate of 50% reported in one series4 and a 2-year survival rate of 35% reported in another.11 Factors associated with increased mortality rates are tumor size, incomplete or no operative resection, and metastatic disease.4 Intracranial malignant fibrous histiocytoma appears to carry a worse prognosis than extracranial or peripheral malignant fibrous histiocytoma. Most patients survive less than 1 year after surgery.3 Other tumors associated with radiation therapy for retinoblastoma, such as osteogenic sarcoma and fibrosarcoma, carry a 1 year survival rate of less than 50%.16
Surgery is the mainstay of therapy for malignant fibrous histiocytoma, and radical rather than conservative excision appears to improve survival times.5,6 The transfacial approach with orbital osteotomy provides wide exposure of the tumor with minimal brain retraction, which helps maximize its resection.2,10 Even with wide local excision, the incidence of recurrence is high. Moderate-dose radiation therapy increases survival times in patients with soft tissue sarcomas and should be considered postoperatively for patients with malignant fibrous histiocytoma.5
References
- Abramson DH, Ellsworth RM, Kitchin FD, et al: Second nonocular tumors in retinoblastoma survivors. Are they radiation-induced?Ophthal-mology 91:1351-1355, 1984
- Beals SP, Joganic EF: Transfacial exposure of anterior cranial fossa and clival tumors. BNI Quarterly 8:2-18, 1992
- Berry AD III, Reintjes SL, Kepes JJ: Intracranial malignant fibrous histiocytoma with abscess-like tumor necrosis. Case report. J Neurosurg 69:780-784, 1988
- Brady MS, Gaynor JJ, Brennan MF: Radiation-associated sarcoma of bone and soft tissue. Arch Surg 127:1379-1385, 1992
- Carabell SC, Goodman RL: Radiation therapy for soft tissue sarcoma. Semin Oncol 8:201-206, 1981
- Cole CH, Magee JF, Gianoulis M, et al: Malignant fibrous histiocytoma in childhood. Cancer 71:4077-4083, 1993
- Escobar-Cuartas F, Antillon-Klussmann F, Alvarez-Morujo-Suarez M, et al: Malignant fibrous histiocytoma of the orbit as second tumor in a case of bilateral retinoblastoma [Spanish]. Bol Med Hosp Infant Mexico 50:745-748, 1993
- Gonzalez-Vitale JC, Slavin RE, McQueen JD: Radiation-induced intracranial malignant fi-brous histiocytoma. Cancer 37:2960-2963, 1976
- Hatashita S, Tajima A, Ueno H: Malignant fibrous histiocytoma in the skull. Case report. Neurol Med Chir (Tokyo) 32:976-979, 1992
- Lawton MT, Hamilton, MG, Beals SP, et al: Radical resection of anterior skull base tumors, in Loftus CM (ed): Clinical Neurosurgery. Baltimore: Williams & Wilkins, 1995, pp 43-70
- Laskin WB, Silverman TA, Enzinger FM: Postradiation soft tissue sarcomas. An analysis of 53 cases. Cancer 62:2330-2340, 1988
- Newton WA Jr., Meadows AT, Shimada H, et al: Bone sarcomas as second malignant neoplasms following childhood cancer.Cancer 67:193-201, 1991
- Nishizawa S, Hayashida T, Horiguchi S, et al: Malignant fibrous histiocytoma of maxilla following radiotherapy for bilateral retinoblastoma. J Laryngol Otol 99:501-504, 1985
- Roarty JD, McLean IW, Zimmerman LE: Inci-dence of second neoplasms in patients with bi-lateral retinoblastoma. Ophthalmology 95:1583-1587, 1988
- Romero FJ, Ortega A, Ibarra B, et al: Post-radiation cranial malignant fibrous histiocytoma studied by CT. Comput Med Imaging Graph 13:191-194, 1989
- Soloway HB: Radiation-induced neoplasms following curative therapy for retinoblastoma. Cancer 19:1984-1988, 1966
