
Clinical Images: Endovascular Occlusion of a Vertebral Artery-Venous Fistula in a Patient with Neurofibromatosis
Authors
Neil M. Borden, MD
Michael T. Lawton, MD†
Cameron G. McDougall, MD†
Robert F. Spetzler, MD†
Judith Santini, MD‡
Divisions of Neuroradiology and † Neurological Surgery, Barrow Neurological Institute, Mercy Healthcare Arizona, Phoenix, Arizona
‡ Department of Anesthesiology, Mercy Healthcare Arizona, Phoenix, Arizona
Key Words : endovascular occlusion, vertebral artery-venous
A 45- year-old male with a history of neurofibromatosis and cervical myelopathy presented with gait disturbance, bilateral finger numbness, and neck pain. A holosystolic bruit was present over the neck. Frontal digital subtraction angiography (DSA) in the early arterial phase after simultaneous injection of both vertebral arteries (Panel A) showed a dysplastic left vertebral artery (arrows). A large fistula (arrowheads) between the left cervical vertebral artery and the adjacent epidural and paravertebral venous plexus had created a vascular steal. Retrograde flow down the upper left vertebral artery from the right vertebral artery with subsequent filling of the fistula was apparent. Frontal DSA in the midarterial phase after bilateral vertebral artery injections (Panel B) showed the fistula filling from above and from below.
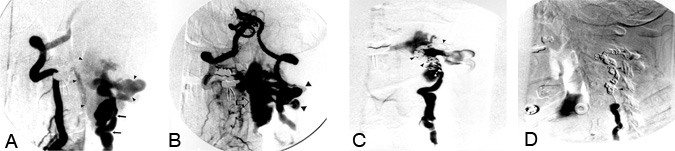
The massively dilated epidural vein (arrow) and the paravertebral venous plexus (large arrowheads) filled early. (The proximal left vertebral artery appears white.) Magnetic resonance imaging (unavailable) showed the dilated epidural vein compressing the cervical spinal cord. Oblique frontal DSA after a left vertebral artery injection during occlusion with endovascular coils (Panel C) showed the multiple platinum microcoils (arrowheads) filling the left vertebral artery just above and at the level of the fistula. Although flow through the fistula was slower, it continued to fill from below.
The final oblique frontal DSA after a left vertebral artery injection (Panel D) showed 38 microcoils (arrowheads) occluding the vertebral artery above, at, and below the site of the fistula, which was obliterated. The patient’s clinical symptoms improved and his neck pain resolved completely. A physical examination performed after the procedure revealed marked improvement in his gait and decreased clonus. Three days after endovascular coil occlusion of the fistula, the patient was discharged.
