
The Practical Use of Magnetic Resonance Angiography for Carotid Endarterectomy: Technical Note
Authors
Jonathan J. Baskin, MD
Adam P. Brown, MD†
Joseph E. Heiserman, MD‡
Robert F. Spetzler, MD
Divisions of Neurological Surgery and Neuroradiology‡ Barrow Neurological Institute, Mercy Healthcare Arizona, Phoenix, Arizona
†Current Address: Coastal Neurosurgical Associates, Wilmington NC
Abstract
The utility of magnetic resonance (MR) angiography in evaluating carotid occlusive disease has been described by multiple authors. This imaging modality is attractive for its reliability, noninvasive nature with no associated morbidity, and relative cost effectiveness. With regard to surgical planning, an advantage of conventional angiography is the ability to localize the level of carotid bifurcation within the cervical region. Typically, this information is inaccessible from the currently generated MR angiographic evaluations. We report a sequence modification with MR angiography that provides this information and assists in surgical planning.
Key Words : carotid endarterectomy, magnetic resonance angiography
Previous communications have reported the accuracy with which magnetic resonance (MR) angiography can be used to define surgically significant carotid occlusive disease.1,5 In those reports, the authors demonstrated the high correlation between MR angiography and duplex ultrasonography or conventional angiography. Additionally, the recently published results of the Asymptomatic Carotid Atherosclerosis Study2 documented a stroke rate of 1.2% due to arteriographic complications during the preoperative evaluation of these patients. The combined morbidity and mortality rate after diagnostic imaging and surgery was 2.7%. At our institution, the evaluation of patients suspected of harboring carotid stenosis now is initiated with MR angiography of the cervical and intracranial vasculature along with standard MR imaging of the brain. Many of the patients referred to us have already undergone evaluation with carotid ultrasonography. We reserve conventional angiography for patients in whom these studies are not definitive.
Whereas the benefits of MR angiographic evaluation include its negligible complication rate, noninvasive nature, and relatively low cost compared to cerebral angiography, preoperative planning for carotid endarterectomy may be more difficult. One reason is that current MR angiography algorithms do not identify the anatomical level of the carotid bifurcation within the cervical region. The carotid bifurcation most commonly occurs at the level of C4-C5 (46.3%), but it also may be found at the extremes of the cervical spine.3 To assist in surgical planning, we report a sequence modification within the MR angiography evaluation that incorporates this easily accessible and important information.
Technique
Two-dimensional time-of-flight MR angiographic images of the neck vessels are generated using the method described by Keller et al.4 A gradient echo-based pulse sequence is used to obtain axial source images with a repetition time (TR) of 48 msec, an echo time (TE) of 8.7 msec, and a flip angle of 60° with fractional echo and first-order flow compensation. A 256 x 128 matrix with one average and acquiring 125 slices of 1.5-mm nominal thickness provide coverage from midcommon carotid artery to the carotid siphon in about 13 min.
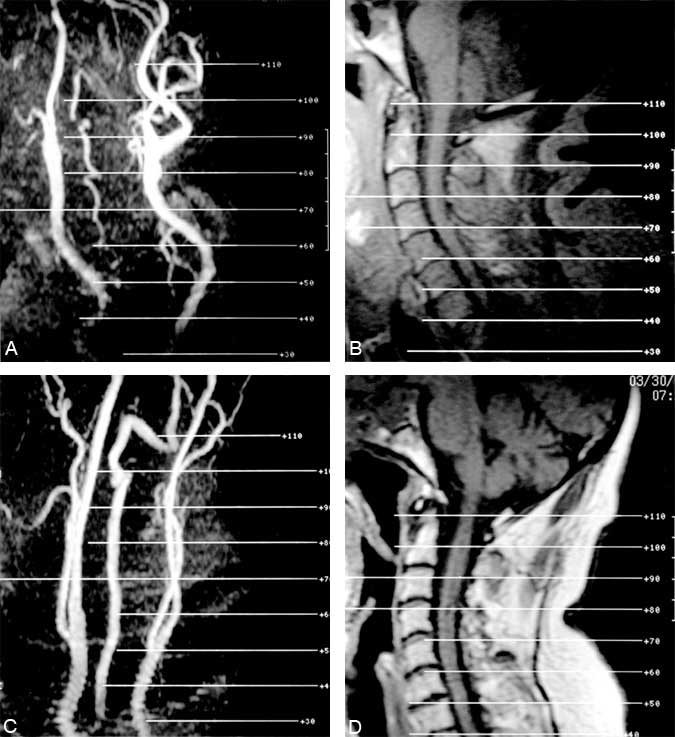
These source images are postprocessed using a maximum intensity pixel algorithm to obtain separate projection images of the left and right sides of the neck at 15° intervals. This process yields 12 projection images spanning 180°. These segmented projection images are printed in multi-image format four on one. The 12 projection images from each side of the neck then occupy six images on a nine-image sheet of film. The remaining three image locations contain the midsagittal T1-weighted localizer of the cervical spine and anteroposterior and oblique bilateral projection images of the neck vessels. These last three images are posted with slice locations so that it is possible to correlate the location of the common carotid bifurcations with the levels of the vertebral bodies (Fig. 1).
Discussion
The two case examples shown in Fig. 1 demonstrate the potential variability in the anatomic location of the carotid bifurcation. Localization with this method is most accurate when referring to the anterior surface of the vertebral body. In these examples, the carotid bifurcation is seen to occur at the C2 level in Patient 1 and at the C6 level in Patient 2. We believe that the described sequence algorithm extends the practical usefulness of MR angiography as this modality evolves toward the primary and, perhaps, sole preoperative imaging study in patients with carotid vascular disease.
References
- Anson JA, Heiserman JE, Drayer BP, et al: Surgical decisions on the basis of magnetic resonance angiography of the carotid arteries. Neurosurgery 32:335-343, 1993
- Executive Committee for the Asymptomatic Carotid Atherosclerosis Study. Endarterectomy for asymptomatic carotid artery stenosis.JAMA 273:1421-1428, 1995
- Huber P: Cerebral Angiography. New York: Thieme Medical, 1982
- Keller PJ, Drayer BP, Fram EK, et al: MR angiography with two-dimensional acquisition and three-dimensional display (work in progress). Radiology 173:527-532, 1989
- Lustgarten JH, Solomon RA, Quest DO, et al: Carotid endarterectomy after noninvasive evaluation by duplex ultrasonography and magnetic resonance angiography. Neurosurgery 34:612-619, 1994
