Impaired Awareness, Finger Tapping, and Rehabilitation Outcome After Brain Injury
George P. Prigatano, PhD
Department of Clinical Neuropsychology, Barrow Neurological Institute, St. Joseph’s Hospital and Medical Center, Phoenix, Arizona
Abstract
Speed of finger tapping after traumatic brain injury has been related to the problem of impaired self-awareness as well as to rehabilitation outcome. This article summarizes selected literature that documents the potentially rich information this “simple” task can provide. It supports Leonard Diller’s emphasis on using developmentally sensitive tasks that allow for simple inferences to be applied to issues of diagnosis and rehabilitation after brain injury.
Key Words: Halstead finger tapping test, impaired awareness, rehabilitation, traumatic brain injury
The professional work and accomplishments of Leonard Diller have demonstrated that psychologists have much to contribute to the rehabilitation and assessment of individuals with traumatic brain injuries (TBIs). An early observation of Diller and Birch8 about accurately appraising children with brain dysfunction has proven to be especially insightful:
“. . . in the main, psychologic tests are not developmentally oriented and the information they supply is discontinuous from age to age. Their interpretation is further complicated by the fact that they consist of contrived situations which are purposefully removed from real life problems. Hence prediction from a given behavior in a test situation to one outside the test situation may involve a complex chain of inferences.” (1964, p. 27)8
A database suggests that speed of finger tapping, as measured by Ward Halstead’s Finger Oscillation Test,12 provides clinically rich information that can be applied to rehabilitation questions with minimal inferences. Curiously, this developmentally sensitive test appears to be related to the clinically and theoretically important problem of impaired self-awareness after brain injury.
The Problem of Impaired Self-Awareness After Brain Injury
At every stage after brain injury, individuals may demonstrate some disturbance in consciousness that affects their ability to perceive accurately or to experience the changes in their cognition and personality that have occurred. This disturbance can be a substantial barrier to successful rehabilitation outcomes.23 That discovery was the impetus for a series of studies aimed at determining how to separate impaired self-awareness as a neuropsychological disturbance from denial of disability as a method of coping. This area of investigation is difficult because it deals with subjective experience as reported verbally by patients.
As Sherlock Holmes comments to Dr. Mortimer, disorders of self-awareness do not constitute a “region of guesswork,” but they do constitute a region . . . “where we balance probabilities and choose the most likely” explanations. “It is the scientific use of the imagination, but we always have some material basis on which to start our speculation.”9 If we are careful observers, we can solve some mysteries that help patients (as well as science) progress.
Impaired Awareness After Brain Injury
Clinicians have observed that the changes in higher cerebral functioning associated with various brain lesions can be related to anosognosia.3,28,37 This phenomenon has always been associated with controversy because it is difficult to describe, classify, and measure. Anosognosia was once described as a generalized effect of dementia, but the work of Anton 1,2 successfully challenged this conception. It has also been described as a psychological defense (i.e., denial of illness), but this view has likewise been reevaluated.29
The outcome of patients treated in a neuropsychologically oriented milieu rehabilitation program 17,19,24 first suggested the importance of this phenomenon. Patients who successfully completed such intensive rehabilitation work often rated their awareness of deficit in a manner similar to the rehabilitation staff who had worked with them for several months. In contrast, patients who had failed treatment universally overestimated their awareness of how their brain injury actually affected their daily behavior (see Table 1 in Prigatano17). These patients tended to minimize the effects of their behavioral and cognitive impairments on their daily function.
Oddy, Coughlan, Tyerman, and Jenkins16 also documented that patients with TBI tended to underestimate their behavioral limitations compared to relatives’ reports. Moreover, 7 years after injury, 40% of relatives described TBI patients as “refusing” to admit to difficulties. The behavior may not be refusal per se but patients’ lack of awareness concerning their specific neuropsychological disturbances.
As a number of studies suggest, the problem of impaired awareness appears to be a disturbance in conscious experience rather than a defense mechanism. These studies attempted to test empirically whether TBI patients would underestimate their behavioral limitations and whether nonneurological factors would influence their self-reports. Prigatano, Altman, and O’Brien21 first tested the hypothesis that patients with severe TBI would underestimate their difficulties in controlling their emotions and behaving in socially appropriate ways. They also predicted that patients would accurately rate their ability to perform self-care activities. The data supported this hypothesis, and the findings were replicated several years later with a new sample of TBI patients.18
Cross-cultural studies, however, suggest that nonneurological factors could also influence self-reports after brain injury. New Zealanders of English ancestry (but not Maori New Zealanders) with a TBI underestimated their behavioral limitations much like American TBI patients.26 A later study with Japanese TBI patients replicated some but not all of the previous findings associated with American TBI patients.27 These discrepancies indicated a need for a multifactorial model to account for the phenomenon of impaired awareness associated with TBI, particularly in young adults with severe TBI.
During the course of these studies, a curious phenomenon was observed: Speed of finger tapping often was slow bilaterally in TBI patients who underestimated their behavioral problems.
Finger Tapping, Severity of Brain Injury, and Disturbances of Self-Awareness
Prigatano and Altman20 classified TBI patients as either overestimating their behavioral competence compared to relatives’ reports or not. Patients who tended to overestimate their behavioral competence (i.e., those with impaired self-awareness) did not differ from other TBI patients on many standardized measures of intelligence or memory. On computed tomography (CT) and magnetic resonance (MR) imaging studies of the brain, however, patients who overestimated their competence had more identifiable lesions than those who did not.
Patients with significant problems with awareness, however, performed slowly on the Halstead Finger Tapping test with both hands although the difference was only statistically significant in the left hand. A cross-cultural study also partially replicated these findings.27 This observation raised the important question of why the speed of finger tapping would relate to this complex neuropsychological disturbance.
Dikmen, Machamer, Winn, and Temkin7 demonstrated that performance on neuropsychological tests often showed a dose-response relationship to the severity of TBI. For example, the correlation between the Revised Halstead Impairment Index score and the median time it took individuals to respond to commands in a purposeful way after TBI was +.59. This observation suggested that severity of TBI was related to level of impairment on complicated neuropsychological measures. Somewhat surprisingly, the Halstead Finger Tapping test showed a similar level of correlation with severity of TBI.
Haaland, Temkin, Randahl, and Dikmen11 found that speed of finger tapping did not recover as well as grip strength after mild to moderate brain injuries. They suggested that this measure may be quite sensitive to the severity of brain injury and therefore would recover less, presumably due to the presence of more diffuse brain damage, even when the initial trauma was considered mild to moderate. Together, these studies suggested that the speed of finger tapping may be a useful marker of severity of TBI and perhaps of the initial level and depth of disturbed consciousness. It may also be a useful measure of recovery (or the lack thereof) and should be assessed serially in TBI patients.
If impaired self-awareness is a neuropsychological disturbance and not a psychiatric impairment, measures of impaired self-awareness should correlate with measures of severity of brain injury as well as with measures of disturbed consciousness as two recent studies suggest.33 First, the correlation between initial Glasgow Coma Scale (GCS) score and clinicians’ rating of patients’ level of awareness several months after TBI is +.39. From the perspective of impairment, Spanish TBI patients demonstrated an identical correlation with admitting GCS score and a measure of impaired self-awareness (i.e., r = -.39).22 These observations led to further hypotheses and speculations.
Postacute TBI patients who show impaired self-awareness often show considerable evidence of disturbed consciousness immediately after brain injury. Patients with a severe TBI may finger tap slowly, presumably because of the diffuseness of their injury. This finding would correlate with a decreased speed of performance.7 Impairments of self-awareness and disorders of speed of finger tapping may therefore be indirectly related. Both dimensions reflect the severity of brain dysfunction. If this is the case, measures of speed of finger tapping as well as measures of impaired awareness should relate to recovery phenomena and rehabilitation outcome.
Speed of Finger Tapping, Rehabilitation Outcome, and Age
Recently, Prigatano and Wong 30 demonstrated that speed of finger tapping was related to rehabilitation out come after an acute unilateral cerebrovascular accident. Interestingly, the speed of finger tapping in the so-called unaffected hand (or hand ipsilateral to the lesion) was most closely associated with achieving rehabilitation goals.
Speed of finger tapping has been also related to employment status after various brain disorders. In a heterogenous group of brain dysfunctional patients, those who were employed full-time tapped at faster rates than unemployed brain dysfunctional persons.13 Perhaps even more interestingly, this simple measure separated full-time from part-time workers.
Dikmen and Morgan6 also reported that individuals with epilepsy who finger tapped slowly tended to be unemployed. Employed patients clearly finger tapped more quickly. In their study, the mean speed of finger tapping in the unemployed epileptic patients was 41 taps/10 sec in the dominant hand and 36 taps/10 sec in the nondominant hand.
Developmental studies show that speed of finger tapping is associated with age. For example, Finlayson and Reitan10 noted that 6-year-old males tend to have a mean speed of finger tapping of 35.6 taps/10 sec with the right hand and 30.0 taps/10 sec with the left hand. Twelve-year-olds tap 41.0 taps/10 sec with the right hand and 36.4 taps/10 sec with the left hand. By age 14, the mean number of taps is 47.3 taps/10 sec with the right hand and 40.7 taps/10 sec with the left hand. Few 14-year-olds, however, are gainfully employed. Individuals seldom obtain and maintain gainful employment at a level that would allow them to be self-sufficient before their late teens or early 20s.
Developmental data show that the mean speed of finger tapping with the dominant hand for individuals between 20 and 39 years old is 49.7 taps/10 sec and 47.0 taps/10 sec with the nondominant hand.4 Between the ages of 40 to 59 years, these rates decline to 42.3 taps/10 sec with the dominant hand and 39.8 taps/10 sec with the nondominant hand. Between the ages of 60 to 69 years, the mean dominant hand speed falls to 39.1 taps/10 sec and to 35.2 taps/10 sec with the nondominant hand.34 It is precisely during this period of life that many individuals seek retirement. Is it possible that speed of finger tapping reflects something general about the overall state of brain function rather than something specific about the sensorimotor strip? Two lines of research suggest that this, in fact, may be the case.
When plotted as a function of age, speed of finger tapping with the right, dominant hand is strikingly parallel with the number of words recalled on the Rey Auditory Learning Test (Fig. 1). The total number of words that individuals are able to recall from age 7 through age 69 parallels almost identically the rate at which they tap on the Halstead Finger Tapping test. These are raw scores, and such strong relationships are rarely found in neuropsychology.34 The findings suggest that the ability to finger tap rapidly is related to important developmental changes, some of which reflect broad, cognitive capacities.
O’Boyle, Gill, Benbow, and Alexander15 reported an incidental but related finding regarding speed of finger tapping and mathematical abilities in right-handed adolescent males. While interested in the question of how verbal problem solving may influence speed of finger tapping in mathematically “gifted” and “average” boys, they found that gifted students finger tapped more rapidly than nongifted students. This study also suggests that speed of finger tapping is related to complex functions and may indicate something about the overall integrity of the brain.
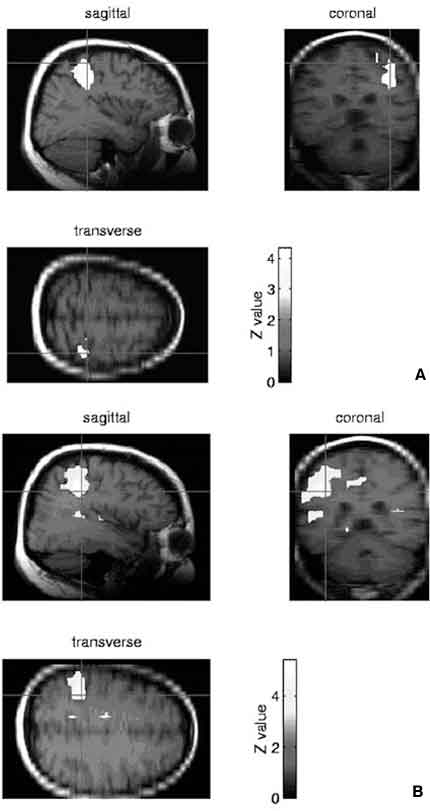
Another way of approaching the relationship of finger tapping to overall brain function is to ask how the relationship changes with time after brain injury. We have begun to explore this issue by measuring functional MR imaging changes in the brain as individuals perform the Halstead Finger Tapping test. In a few case studies done at our institution, individuals showed bilateral activation when performing this simple task. In a recent case study, Sterling Johnson at Dartmouth (personal communication, 1999) further documented this phenomenon using more precise methodology (Fig. 2). His case example illustrates that while activation is increased in the parietal and sensorimotor area, there is often evidence of bilateral activation in individuals performing this simple task. This activation occurs when both the right and left hand perform the task. Thus, two lines of research suggest that the Halstead Finger Tapping test is quite sensitive to more than the integrity of the sensorimotor strip. Performing this task requires both initiatory and inhibitory controls. It appears to be related to complex cognitive functions reflected in dynamic changes in cerebral blood flow.
Finger Movements and Recovery and Deterioration
Studies of recovery of function by Frackowiak and others5,35,36 have also shown that when individuals recover from incapsular infarctions, as measured by simple movement of fingers, the cerebral hemispheres are often activated bilaterally. This activation is often far removed from the site of the lesion and includes the frontal and parietal regions. The implication is that when motor function recovers, even after a small lesion in subcortical structures, the entire brain may become activated in order for a relatively simple function such as finger tapping to approach normal limits.
Studies of deterioration have also found speed of finger tapping to be a sensitive measure. Compared to age-matched controls, patients with early stage dementia of the Alzheimer’s type tap significantly slower (and less accurately).14 Activation of the brain is widespread when patients with cerebellar degeneration performed a self-paced sequential finger movement task.38 This nontapping but sequential finger movement activity causes bilateral activation in the prefrontal cortex, inferior parietal lobe, putamen, and cerebellum. The authors concluded that “the reduced activity of the cerebellar neurons in the patients produced a complex pattern of rCBF (regional cerebral blood flow) increases and decreases in other brain regions” (p. 379).
Simple finger movements at various stages of recovery and deterioration may actually reflect dynamic brain activity (or the lack of it). It may be for this reason that speed of finger tapping relates not only to rehabilitation outcome and employability after brain lesions but to the important emergent brain function of self-awareness.
Self-Awareness and Rehabilitation Outcome
Recently, Sherer, Bergloff, Levin, High, Ogden, and Nick32 studied the relationship between impaired awareness and employment outcome after TBI using multiple regression analysis. They studied this variable in terms of five other important variables: severity of initial brain injury, chronicity of brain injury, the patient’s employment status before injury, the patient’s history of alcohol use before injury, and the patient’s level of cognitive functioning from admission through postacute brain injury rehabilitation. Two measures of impaired self-awareness correlated as strongly in predicting employment outcome as did any of these factors (Table 1). The findings provide objective evidence confirming clinical observations of brain dysfunctional patients during the last 15 to 20 years.
Prigatano and Wong31 studied how various higher cerebral functions relate to rehabilitation outcome after acute brain injury. Patients who could accurately predict their ability to recall three words with distraction (a measure of self-awareness?) were much more likely to achieve rehabilitation goals than individuals who were unable to predict their performance accurately. Patients who showed improvement in spontaneous affect were more likely to achieve their rehabilitation goals. These findings are of considerable theoretical interest because self-awareness has been defined as an emergent brain function that by its nature integrates “thinking” and “feeling.”19 Thus, both cognitive and affective functioning would be expected to improve in patients whose self-awareness improves.
Consequently, it may be helpful to distinguish different forms of impaired self-awareness and how they relate to denial of disability.
Different Forms of Impaired Self-Awareness and Denial of Disability
The research reviewed above, as well as other studies,19 has led to a reevaluation of certain clinical observations. The earlier notion that “impaired self-awareness” represents a neuropsychological disturbance and “denial of disability” represents a psychiatric disturbance must be abandoned.25 As Prigatano and Schacter28 have noted, different forms of self-awareness seem to emerge after different types of brain insults. Depending on the region of the brain that is damaged, different disorders of self-awareness may emerge.
Four syndromes of self-awareness can be identified:19 frontal heteromodal, parietal heteromodal, temporal heteromodal, and occipital heteromodal syndromes. When the frontal heteromodal regions are damaged, individuals’ awareness of socially inappropriate actions may be impaired or they may lack awareness about disorders of planning, initiation, and so on. When the parietal heteromodal regions are damaged, individuals’ awareness of a limb (classic anosognosia for hemiplegia) is often disturbed as well as apraxic disturbances. Temporal heteromodal syndromes are associated with a wide variety of impairments in awareness that can include poor awareness of language dysfunction and memory impairments. Occipital heteromodal syndromes are often associated with disturbances in the awareness of loss of vision.
Bilateral cerebral dysfunction often produces complete syndromes. When brain dysfunction is primarily unilateral, these syndromes may be partial (much like aphasic syndromes). Different methods of coping emerge in individuals with partial unawareness.
Certain methods of coping can be described as nondefensive while others can be described as defensive. Nondefensive methods of coping involve individuals using the same methods to deal with problems after injury as they used before injury. For example, a university professor may insist that he can return to his job after a right hemispheric stroke because work has always been the way in which he has organized his life and obtained his primary sense of value. In contrast, other individuals may insist that they can return to work because they cannot tolerate the notion that they have any impairment whatsoever. Such individuals often accuse therapists of purposely blocking them from accomplishing their goals. This situation represents a defensive maneuver, and almost any form of defense mechanism might be used. In fact, the defenses frequently go beyond denial and include projection, which can lead to substantial distortions of reality and often to the development of delusions several years after brain injury.19
When neuropsychologists are confronted with patients with complete or partial syndromes of impaired self-awareness, they must understand what patients actually experience. As clinicians enter a patient’s phenomenological field, they are better able to determine what level of rehabilitation the patient can, in fact, engage. If patients have a complete syndrome of unawareness, they will have little if any motivation to engage in rehabilitation. They seldom resist rehabilitation but simply participate passively. Individuals with partial syndromes of impaired awareness are less likely to be compliant. Those who use nondefensive methods of coping to deal with their impaired awareness often cooperate as they slowly begin to recognize that their impairments preclude them from doing a variety of activities. The neuropsychological rehabilitation program described by Prigatano and colleagues24 has been most successful with this subgroup of patients. When individuals use defensive methods of coping (e.g., use denial, projection), they are much more difficult to involve in a milieu-oriented program. Such individuals may need individual psychotherapy before they can tolerate discussion and recognition of their disabilities.19
Conclusions
Leonard Diller’s contribution to the rehabilitation of brain dysfunctional patients has been substantial. In his early writings, he encouraged psychologists to explore developmentally sensitive measures of brain function that would permit inferences concerning real-world functioning. The Halstead Finger Tapping test may meet this criterion, at least, for patients with severe TBI. It is sensitive to the severity of initial injury and disturbances of consciousness, to later measures of impaired awareness, and to rehabilitation outcome. It changes predictably with age and correlates with such complex functions as rote verbal learning across the life span.
Rehabilitation psychologists and neuropsychologists can use this measure and the large literature supporting it to improve inferences about patients’ level of functioning and disability. Following the model and spirit of Leonard Diller’s work, they can use the most parsimonious ways of understanding patients’ behavior to build on these observations methods of rehabilitation, which are practical and substantially improve the quality of patients’ lives.
An earlier version of the paper was presented as the First Leonard Diller Honorary Lecture of Division 22, American Psychological Association Meeting, August 16, 1998 in San Francisco, CA. From Prigatano, GP: Impaired awareness, finger tapping, and rehabilitation outcome after brain injury. Rehab Psychol 44:145-159, 1999. Copyright © 1999 by the Educational Publishing Foundation. Adapted with permission. ”
References
- Anton G: Blindheit nach beiderseitiger Gehirnerkrankung mit Verlust der Orientierung in Raume. Mittherlungen des Vereines der Arzte in Steiermark 33:41-46, 1896
- Anton G: Ueber herderkrankungen des Gehirnes, welche von Patientsen selbst nicht wahrgenommen werden. Wien Klin Wchnschr 11:227-229, 1898
- Bisiach E, Geminiani G: Anosognosia related to hemiplegia and hemianopia, in Prigatano GP, Schacter RL (eds): Awareness of Deficit After Brain Injury. Clinical and Theoretical Issues. New York: Oxford University, 1991, pp 17-39
- Bornstein RA: Normative data on selected neuropsychological measures from a nonclinical sample. J Clin Psychol 41:651-659, 1985
- Chollet F, DiPiero V, Wise RJS, et al: The functional anatomy of motor recovery after stroke in humans: A study with positron emission tomography. Ann Neurol 29:63-71, 1991
- Dikmen S, Morgan SF: Neuropsychological factors related to employability and occupational status in persons with epilepsy. J Nerv Ment Dis 168:236-240, 1980
- Dikmen SS, Machamer JE, Winn HR, et al: Neuropsychological outcome at 1-year post head injury. Neuropsychology 9:80-90, 1995
- Diller L, Birch HG: Psychological evaluation of children with cerebral damage, in Birch HG (ed): Brain Damage in Children. The Biological and Social Aspects. Baltimore: Williams & Wilkins, 1964
- Doyle AC: Sherlock Holmes: The Complete Novels and Stories. New York: Bantam, 1986
- Finlayson MA, Reitan RM: Handedness in relation to measures of motor and tactile-perceptual function in normal children. Percept Mot Skills 42:475-481, 1976
- Haaland KY, Temkin N, Randahl G, et al: Recovery of simple motor skills after head injury. J Clin Exp Neuropsychol 16:448-456, 1994
- Halstead WC: Brain and Intelligence. Chicago: University of Chicago, 1947
- Heaton RK, Chelune GJ, Lehman RAW: Using neuropsychological and personality tests to assess the likelihood of patient employment. J Nerv Ment Dis 166:408-416, 1978
- Müller G, Weisbrod S, Klingberg F: Finger tapping frequency and accuracy are decreased in early stage primary degenerative dementia. Dementia 2:169-172, 1991
- O’Boyle MW, Gill HS, Benbow CP, et al: Concurrent finger-tapping in mathematically gifted males: Evidence for enhanced right hemisphere involvement during linguistic processing. Cortex 30:519-526, 1994
- Oddy M, Coughlan T, Tyerman A, et al: Social adjustment after closed head injury. A further follow-up seven years after injury. J Neurol Neurosurg Psychiatry 48:564-568, 1985
- Prigatano GP: Disturbances of self-awareness of deficit after traumatic brain injury, in Prigatano GP, Schacter DL (eds): Awareness of Deficit After Brain Injury. Clinical and Theoretical Issues. New York: Oxford University, 1991, pp 111-126
- Prigatano GP: Behavioral limitations TBI patients tend to underestimate: A replication and extension to patients with lateralized cerebral dysfunction. The Clinical Neuropsychologist 10:191-201, 1996
- Prigatano GP: Principles of Neuropsychological Rehabilitation. New York: Oxford University, 1999
- Prigatano GP, Altman IM: Impaired awareness of behavioral limitations after traumatic brain injury. Arch Phys Med Rehabil 71:1058-1064, 1990
- Prigatano GP, Altman IM, O’Brien KP: Behavioral limitations that traumatic-brain-injured patients tend to underestimate. The Clinical Neuropsychologist 4:163-176, 1990
- Prigatano GP, Bruna O, Mataro M, et al: Initial disturbances of consciousness and resultant impaired awareness in Spanish patients with traumatic brain injury. J Head Trauma Rehabil 13:29-38, 1998
- Prigatano GP, Fordyce DJ, Zeiner HK, et al: Neuropsychological rehabilitation after closed head injury in young adults. J Neurol Neurosurg Psychiatry 47:505-513, 1984
- Prigatano GP, Fordyce DJ, Zeiner KH, et al: Neuropsychological Rehabilitation After Brain Injury. Baltimore: Johns Hopkins University, 1986
- Prigatano GP, Klonoff PS: A clinician’s rating scale for evaluating impaired self-awareness and denial of disability after brain injury. The Clinical Neuropsychologist 11:1-12, 1997
- Prigatano GP, Leathem JM: Awareness of behavioral limitations after traumatic brain injury: A cross-cultural study of New Zealand Maoris and Non-Maoris. The Clinical Neuropsychologist 7:123-135, 1993
- Prigatano GP, Ogano M, Amakusa B: A cross-cultural study on impaired self-awareness in Japanese patients with brain dysfunction. Neuropsychiatry Neuropsychol Behav Neurol 10:135-143, 1997
- Prigatano GP, Schacter DL: Awareness of Deficit After Brain Injury. Clinical and Theoretical Issues. New York: Oxford University, 1991
- Prigatano GP, Weinstein EA: Edwin A. Weinstein’s contributions to neuropsychological rehabilitation. Neuropsychological Rehabilitation 6:305-326, 1996
- Prigatano GP, Wong JL: Speed of finger tapping and goal attainment after unilateral cerebral vascular accident. Arch Phys Med Rehabil 78:847-852, 1997
- Prigatano GP, Wong JL: Cognitive and affective improvement in brain dysfunctional patients who achieve inpatient rehabilitation goals. Arch Phys Med Rehabil 80:77-84, 1999
- Sherer M, Bergloff P, Levin E, et al: Impaired awareness and employment outcome after traumatic brain injury. J Head Trauma Rehabil 13:52-61, 1998
- Sherer M, Boake C, Levin E, et al: Characteristics of impaired awareness after traumatic brain injury. J Int Neuropsychol 4:380-387, 1998
- Spreen O, Strauss E: A Compendium of Neuropsychological Tests. Administration, Norms, and Commentary. New York: Oxford University, 1991
- Weiller C, Chollet F, Friston KJ, et al: Functional reorganization of the brain in recovery from striatocapsular infarction in man. Ann Neurol 31:463-472, 1992
- Weiller C, Ramsay SC, Wise RJS, et al: Individual patterns of functional reorganization in the human cerebral cortex after capsular infarction. Ann Neurol 33:181-189, 1993
- Weinstein EA, Kahn RL: Denial of Illness. Symbolic and Physiological Aspects. Springfield, IL: Charles C Thomas, 1955
- Wessel K, Zeffiro T, Lou J-S, et al: Regional cerebral blood flow during a self-paced sequential finger opposition task in patients with cerebellar degeneration. Brain 118:379-393, 1995