
Bow Hunter’s Stroke
G. Michael Lemole, Jr, MD
Jeffrey S. Henn, MD
Robert F. Spetzler, MD
Joseph M. Zabramski, MD
Division of Neurological Surgery, Barrow Neurological Institute, St. Joseph’s Hospital and Medical Center, Phoenix, Arizona
Abstract
Bow hunter’s stroke is characterized by vertebrobasilar insufficiency caused by occlusion or stenosis of the vertebral artery associated with head movements. The compromised blood flow is usually conditional upon an isolated posterior circulation with a hypoplastic, stenotic, or occluded contralateral vertebral artery and little input from the anterior circulation via the circle of Willis. The signs and symptoms of vertebrobasilar insufficiency range from dizziness, nystagmus, and nausea and vomiting to frank hemiparesis, sensory changes, Horner’s syndrome, swallowing difficulties, and loss of consciousness. Symptoms may be transient in the case of temporarily compromised blood flow or may persist when insufficient blood flow or resulting embolus or thrombus produce an infarction in the affected vascular territory. The extracranial vertebral artery usually becomes occluded when the head is rotated while the artery is fixed by surrounding bony or fibrous structures. Diagnosis usually requires dynamic studies that measure absolute or relative changes in cerebral blood flow as a result of head movement; angiography is considered the gold standard. Treatments range from conservative warnings to minimize head movement to surgical procedures designed to limit head rotation or to decompress and free the vertebral artery at the point of compression. Because the risk of a cerebrovascular accident with permanent sequela from this syndrome is significant, some form of intervention should be instituted. Patients’ medical conditions and expectations should be weighed against the severity of the disease when choosing among surgical options.
Key Words: bow hunter’s stroke, vertebrobasilar insufficiency
Bow hunter’s stroke has been defined as “hemodynamic vertebral basilar insufficiency induced by forced or voluntary rotational head movements causing intermittent vertebral artery compression at the atlanto axial level.”[7] Although the term “stroke” is used throughout the literature to refer to the condition, bow hunter’s encompasses a wide spectrum of rotational hemodynamic insuffiency ranging from a transient ischemic attack (TIA) to a frank cerebrovascular accident (CVA). As the predisposing factors, mechanisms, and pathophysiology underlying this condition have become more widely understood, more treatment options have become available. The current options of conservative treatment, surgical fusion, or vertebral artery decompression must be weighed against patients’ medical condition and personal desires. This article presents two case illustrations and reviews the natural history, diagnosis, and treatment of bow hunter’s stroke.
Illustrative Cases
Case 1
A 71-year-old Caucasian female sought treatment after experiencing nausea and vertigo for 3 months. The nausea had been followed by difficulty with vision and loss of consciousness. These symptoms occurred when the patient turned her head to the right and were aggravated when she extended her head. She became dizzy when looking up into her cupboards and shelves. The patient’s medical history was remarkable only for hypertension, which had developed about 3 years earlier and was being treated pharmacologically.
On neurological examination, the patient appeared to be fully alert and oriented. Her cranial nerve function was intact, and her motor and sensory function was normal. The diagnosis of positional syncope was suspected.
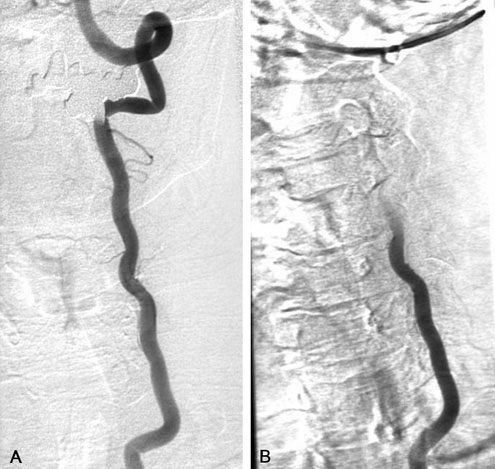
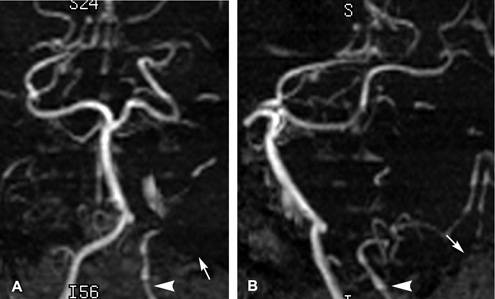
Angiographic injection of the right vertebral artery revealed an occlusion from the vessel’s origin to its midcervical region. Injection of the common carotid arteries showed no evidence of blood flow through the posterior communicating arteries (PCoAs) into the posterior circulation. When the patient turned her head to the right, a transient occlusion of the left vertebral artery was observed (Fig. 1). She experienced a TIA during which she lost consciousness; she stopped breathing and her pupils dilated. When the patient’s head was returned to midline, normal blood flow through the left vertebral artery resumed and her symptoms abated. The occlusion was attributed to mechanical compromise of the artery at C1.
The patient underwent decompression of the left vertebral artery with hemilaminectomy at C1. The vertebral artery was completely freed from the sulcus arteriosus. The patient’s postoperative course was unremarkable, and she remained neurologically intact. She wore a soft cervical collar during the immediate postoperative period and has experienced no further symptoms. A follow-up angiogram obtained 3 months after surgery revealed no evidence of vertebral compromise with rotation of the head.
Case 2
A 71-year-old Caucasian male sought treatment for dizziness, which occurred reproducibly, when he turned his head to the right and when he bent his head forward while playing golf. For fear of losing consciousness, he had voluntarily limited rotatory movements of his head. Previously, he had undergone bilateral carotid endarterectomies and had a history of hyperlipidemia, hypothyroidism, osteoarthritis, and an occlusion of the right central vein. His medications included clopidogrel bisulfate and aspirin.
The patient’s neurological examination was nonfocal except for a minor bilateral loss of hearing. All other cranial nerve function was intact, and motor, sensory, cerebellar, and long-tract signs were also within normal limits.
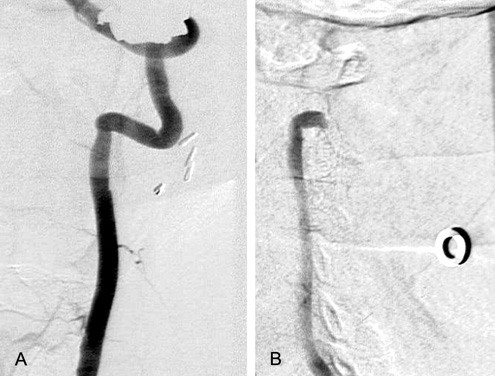
Vertebral angiographic injections demonstrated chronic occlusion of the right vertebral artery. On carotid injection, the vertebrobasilar system failed to backfill through the PCoAs. When the patient’s head was turned to the right, the left vertebral artery occluded transiently (Fig. 2A), but no symptoms manifested during the examination.
Given the patient’s isolated posterior circulation and the presence of symptoms despite coincidental antiplatelet therapy, vertebral artery decompression was recommended. The patient chose to undergo a posterior approach for decompression of the left vertebral artery with a left-sided C1 hemilaminectomy. Postoperatively, dynamic angiography demonstrated normal blood flow through the left vertebral artery when his head was turned. The patient has experienced no further symptoms.
Discussion
The association between head rotation and vertebral artery compromise, particularly on the side contralateral to head rotation, was first noted in cadaveric studies.[20] Individual case histories and, ultimately, dynamic cerebral angiography further related vertebrobasilar insufficiency to vertebral artery compromise.[7,9-12,18,22]
In 1933 DeKleyn and Versteegh[4] first described vertigo and nystagmus produced by head movement. In autopsy studies, they noted compromise of the contralateral vertebral circulation when the head was turned to one side. In 1947 Pratt-Thomas and Berger[16] revealed a closer association between head position and compromise of the vertebral artery in three patients who died after chiropractic manipulation of the neck. In autopsy studies, Ford and Clark[6] found thrombus in the basilar artery of two patients who had undergone neck manipulation and who had experienced vertigo, nausea, and hemiparesis before they died. The authors suggested that the patients most likely suffered compromised blood flow in the extracranial vertebral artery at the point of rotation between the atlas and the axis and surmised that this event resulted in distal thrombosis.
Ford[5] later described a 17-year-old male who could produce signs and symptoms of vertebrobasilar insufficiency with voluntary head movements. His evaluation revealed a dens defect at C2. The patient was thought to have abnormal mobility at C1-C2; fusion at that level completely relieved his symptoms. Biemond[3] also reported patients who exhibited signs and symptoms of compromised blood flow in the posterior circulation with rotational head movements and who ultimately were found to have basilar artery thrombosis.
Tatlow and Bammer[20] described three more patients with posterior circulation symptoms referable to head movements who appeared to have suffered CVAs as a result of their compromised blood flow. All three patients were treated with anticoagulation therapy without recurrent strokes. In separate cadaveric studies, the authors showed that blood flow in the contralateral vertebral artery was interrupted when the head was rotated to one side. Numerous authors have since used cerebral angiography to document vertebral artery compromise resulting from head rotation.[2,7,10,11,15,18]
In 1978 Sorensen[19] coined the term “bow hunter’s stroke” to describe the sudden onset of right-sided hemi paresis, contralateral hemisensory changes, and a dilated right pupil in a 39-year-old man after he turned his head during archery practice. The patient was thought to have Wallenberg’s syndrome from lateral medullary infarction. Vertebral angiography revealed spasm in the right vertebral artery while the left vertebral artery was normal. Sorensen surmised that the right vertebral artery had been compromised when the patient turned his head to the left. Sluggish blood flow through the right posterior inferior cerebellar artery (PICA) with possible emboli or thrombosis of distal vascular territories then caused brain stem and cerebellar symptoms. The patient survived with persistent neurological deficits. Since Sorensen’s report,19 additional series have described patients with bow hunter’s stroke who presented with either a completed stroke or TIA referable to changes in head position.[7,9-12,18,22]
Incidence and Epidemiology
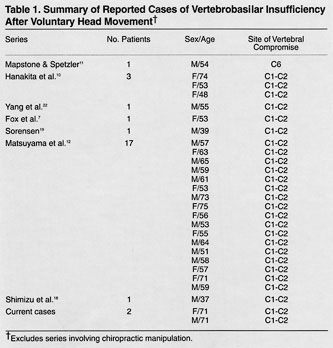 Because of the relative rarity of bow hunter’s stroke, exact figures regarding its incidence and prevalence by age and sex are unavailable. The three patients described by Tatlow and Bammer[20] were more than 60 years old, and angiographic studies were not obtained. Sorensen’s case[19] involved a 39-year-old male. The age and sex distribution of the individual case reports of vertebrobasilar insufficiency with voluntary head movements are shown in Table 1.
Because of the relative rarity of bow hunter’s stroke, exact figures regarding its incidence and prevalence by age and sex are unavailable. The three patients described by Tatlow and Bammer[20] were more than 60 years old, and angiographic studies were not obtained. Sorensen’s case[19] involved a 39-year-old male. The age and sex distribution of the individual case reports of vertebrobasilar insufficiency with voluntary head movements are shown in Table 1.
Frisoni and Anzola[8] compiled 36 cases from the literature as well as three of their own to examine the subset of patients who experienced vertebrobasilar ischemic strokes after chiropractic manipulation. In their series, the male-to-female distribution was about equal and the mean age was about 39 years. Clinical syndromes were referable to strokes in the following distributions: 5% occipital lobe, 8% cerebellar, 8% locked-in syndrome, 28% Wallenberg’s syndrome, 49% other brain stem, and 2% unclassified. The long-term impairment or mortality rate associated with these injuries was 28%, underscoring the devastating consequences that can be associated with CVAs caused by neck manipulation.
In contrast to the series compiled by Frisoni and Anzola,8 voluntary head rotation rather than forced external neck manipulation induced signs and symptoms of bow hunter’s stroke in a surgical series by Matsuyama et al.[12] Their patients (10 males and 7 females) were older (mean age, 60 years) than those in Frisoni’s and Anzola’s series. Furthermore, none of these patients were diagnosed with fixed deficits or strokes as were all of Frisoni’s and Anzola’s[8] cases.
Mechanism and Pathophysiology
In most studies, head rotation occludes the vertebral artery at the junction of C1-C2. The predominance of this site for occlusion is accounted for by the immobilization of the vertebral artery at the transverse foramina of C1 and C2 and along the sulcus arteriosus to where it inserts into the dura. However, sites other than the atlantoaxial level can be the source of vertebral artery compression with head rotation.[9,11] Mapstone and Spetzler[11] described a fibrous band anchoring the vertebral artery just before its entrance into the transverse foramen at C6. Head turning occluded the artery at the level of the fibrous band, and surgical sectioning of the band eliminated the symptoms.
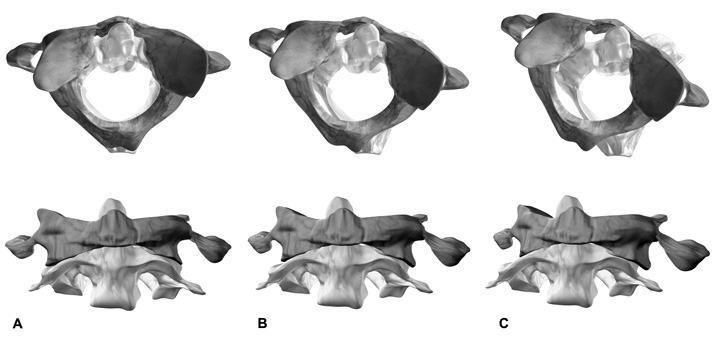
Biomechanical studies of neck rotation[1,21] demonstrate that the contralateral atlantoaxial joint rotates asymmetrically forward and downward as a result of head turning (Fig. 3)
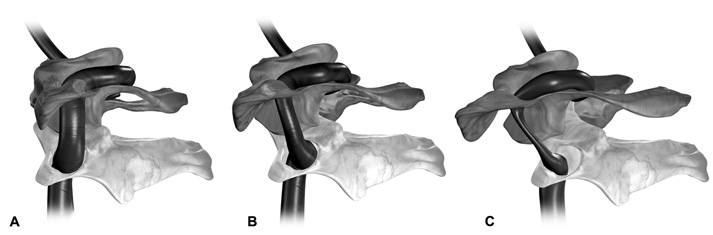
The contralateral vertebral artery may be stretched between its points of fixation either between C1 and C2 (Fig. 4) or as it runs under the atlanto-occipital ligament along the posterior ring of C1. Stretching and compromise of the contralateral vertebral artery may even be a normal physiological variant.
Most people with a compromised vertebral artery never become symptomatic because cerebrovascular redundancy is provided by a healthy contralateral vertebral artery, adequate blood flow from the anterior circulation through anastomoses at the circle of Willis, or both.[20] In fact, the common underlying feature of most cases of bow hunter’s stroke is an isolated posterior circulation. Isolation of the posterior circulation requires one of the vertebral arteries to be insufficient.
The insufficiency may reflect a congenital anomaly, as in the case of hypoplastic vertebral arteries or those that terminate in PICA (Fig. 5). Interestingly, Sorensen’s patient appeared to have a healthy vertebral artery opposite the vessel affected by head turning.[19]
Ultimately, bow hunter’s stroke encompasses a spectrum of causes for vertebrobasilar insufficiency, ranging from mechanical obstruction of the vertebral artery with a resultant TIA to vertebral artery compromise and possible injury with resulting embolus, thrombosis, and infarction. Spondylotic bone spurs, particularly along the foramen transversarium, can cause intermittent vertebral artery compression with head rotation.[13,17] Compromise of the vertebral artery can also be acquired as is the case with atherosclerotic disease. External compression from tumors, osteophytes, fibrous bands, infectious processes, or trauma can narrow or anchor the vertebral artery.[9] Trauma to the vertebral artery can also cause occlusions,[1] leaving patients susceptible to a bow hunter’s stroke if the head is rotated away from the remaining patent vertebral artery.
Recently, Pamphlett et al.[14] suggested that sudden infant death syndrome and rotational vertebral artery compression were associated. Postmortem examinations revealed bilateral vertebral artery compression between the occipital bone and C1 in three of five infants found with head extension. In nine cases where neck rotation was noted, vertebral artery compression was described in three. The authors surmised that inadequate collateral blood flow along with the symptomatic compression of the vertebral artery(s) could have caused a fatal infarction.
Diagnosis
A history of vertebrobasilar symptoms referable to a particular head position must be considered highly suspicious for the diagnosis of bow hunter’s stroke. Tatlow and Bammer[20] described a series of maneuvers on a Stryker bed to isolate symptoms caused by head positioning relative to the torso from those caused by head positioning alone. The maneuvers were intended to distinguish traditional vestibular system- associated vertigo and nausea from symptoms related to vascular compromise.
Cerebral angiography provides the causative link between vertebral artery compression and a patient’s symptoms by demonstrating compromised blood flow in the referable vessels with head rotation. The affected vertebral artery may appear normal when the head is held in the neutral position. Carotid injections can help demonstrate cross-filling of the posterior circulation through the PCoAs or fetal variant anastomoses between the two circulations. During trial dynamic cerebral angiography, simple turning of the neck can have immediate and drastic consequences as in Case 1 or no noticeable effects as in Case 2.
Computed tomographic (CT) angiography may be particularly useful in demonstrating the vertebral artery and its relation to surrounding bony elements. Matsuyama et al.[12] provided a compelling CT angiographic view of a vertebral artery being stretched between the transverse foramina of C1 and C2 when the head was turned to the contralateral side. These authors further recommended the use of single photon emission CT to demonstrate deficiencies in cerebral blood flow in the posterior fossa when the head is turned. These deficiencies should correlate with the distribution of the compromised vertebral artery.
Because cerebral angiography is associated with a risk of stroke, less invasive diagnostic modalities such as CT angiography and spectrography may become more accepted for the diagnosis of bow hunter’s stroke in the future. The decision to proceed with more invasive diagnostic procedures must be related to patients’ deficits and symptoms and their reproducibility with head positioning.
Treatment and Outcomes
Patients with bow hunter’s stroke have been treated conservatively with anticoagulation therapy.[20] Other noninvasive approaches have included encouraging the patient not to turn the head to the affected side or the use of a cervical collar to provide a palpable reminder. Fearing that symptoms will return or that they will lose consciousness, many patients find this form of treatment unacceptable.
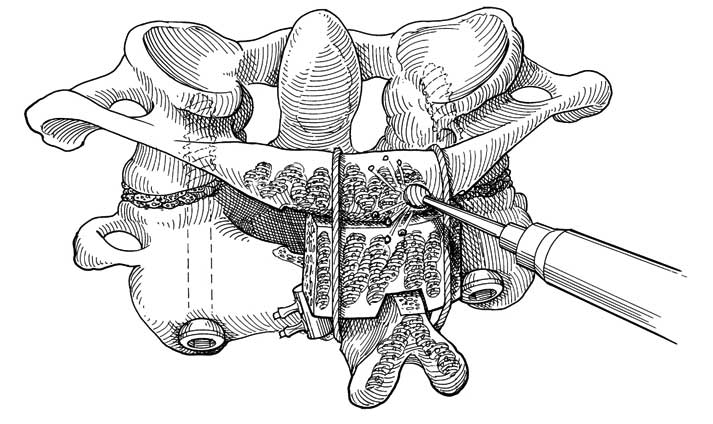
When symptoms are caused by rotation at C1-C2, a logical surgical approach is to perform a fusion and fixation at that level (Fig. 6).[5,22] Fusion at C1-C2 has been associated with resolution of symptoms.[5,12,22] The disadvantage of this approach, however, is that neck rotation can be limited by as much as 50% to 70%.[12] In one series, patients whose rotational movements were extremely reduced experienced significant discomfort. Overall, however, the patients were satisfied with the surgery because the symptoms of bow hunter’s stroke did not return.[12]
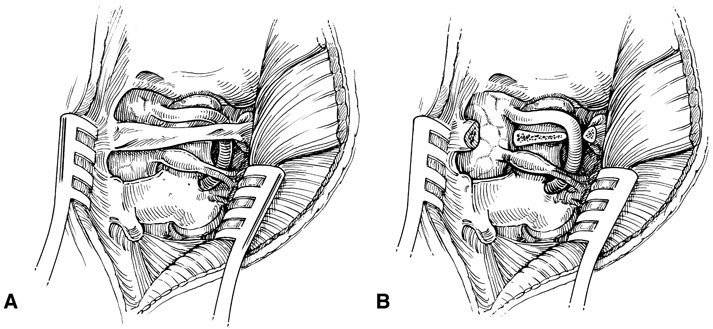
An alternate treatment is surgical decompression of the vertebral artery. Shimizu et al.[18] used a posterior approach to the arch of C1 (Fig. 7) to release the vertebral artery from its fixation points in the transverse foramen and sulcus arteriosus by performing a hemilaminectomy. Patients exhibited no further symptoms after surgery, and no rotary obstruction was apparent at that level on postoperative angiography. Surgical intervention to decompress fibrous bands[11] or osteophytic spurs[13,17] appears to offer long-term relief from symptoms, but no large series are available. Other approaches, including the anterolateral approach for decompression of the atlantoaxial vertebral artery, have also been described.[7]
Matsuyama et al.[12] compared the efficacy of C1-C2 posterior fusion in eight patients to decompression of the vertebral artery alone in nine patients. Range of motion was reduced in those who underwent surgical fusion, but their symptoms did not recur. Conversely, of the nine patients who underwent vertebral artery decompression alone, three (33%) patients experienced recurrent symptoms and subsequently underwent surgical fusion. In these patients, dynamic angiography showed that the vertebral artery on the operated side was still occluded with head rotation. One patient developed a right cerebellar infarction between operations.
Although it is unclear which operation should be performed initially, Matsuyama et al.[12] concluded that to avoid vertebral artery occlusion with certainty a posterior fusion should be considered. Routinely assessing the efficacy of decompression with cerebral angiography in the postoperative period was not mentioned. As our cases demonstrate, decompression of the vertebral artery alone can provide excellent symptomatic relief and can be assessed with cerebral angiography after surgery. The senior authors (RFS and JMZ) use posterior decompression of the vertebral artery as a first-line surgical therapy to avoid compromising cervical range-of-motion. Postoperative dynamic angiography readily tests surgical efficacy. If patients subsequently fail clinically or on diagnostic evaluation, a stabilization and fusion procedure is considered. If surgery for bow hunter’s stroke is to be entertained, patients must be informed of the advantages and disadvantages of each procedure.
Conclusion
As with epidemiological data regarding bow hunter’s stroke, the long-term outcome of patients with this disease is not clearly understood given the overall rarity of the condition. But, because bow hunter’s stroke is caused by mechanical obstruction of the vertebral artery with neck rotation, any intervention that alleviates the compression and restores blood flow should significantly improve outcomes.
References
- Barton JW, Margolis MT: Rotational obstructions of the vertebral artery at the atlantoaxial joint. Neuroradiology 9:117-120, 1975
- Bauer RB: Mechanical compression of the vertebral arteries, in Berguer R, Bauer RB (eds): Vertebrobasilar Arterial Occlusive Disease. Medical and Surgical Management. New York: Raven Press, 1984, pp 45-71
- Biemond A: Thrombosis of basilar artery and vascularization of brain stem. Brain 74:300-317, 1951
- DeKleyn A, Versteegh C: Uber verschiedene formen von nemieres syndrom. Deutsche Ztschr Nervenh 132:157-189, 1933
- Ford FR: Syncope, vertigo and disturbances of vision resulting from intermittent obstruction of vertebral arteries due to defect in odontoid process and excessive mobility of second cervical vertebra. Bull Johns Hopkins Hosp 91:168-173, 1952
- Ford FR, Clark D: Thrombosis of the basilar artery with softenings in the cerebellum and brain stem due to manipulation of the neck; a report of two cases with one post-mortem examination, reasons are given to prove that damage to the vertebral arteries is responsible. Bull Johns Hopkins Hosp 98:37-42, 1956
- Fox MW, Piepgras DG, Bartleson JD: Anterolateral decompression of the atlantoaxial vertebral artery for symptomatic positional occlusion of the vertebral artery. Case report. J Neurosurg 83:737-740, 1995
- Frisoni GB, Anzola GP: Vertebrobasilar ischemia after neck motion. Stroke 22:1452-1460, 1991
- George B, Laurian C: Impairment of vertebral artery flow caused by extrinsic lesions. Neurosurgery 24:206-214, 1989
- Hanakita J, Miyake H, Nagayasu S, et al: Angiographic examination and surgical treatment of bow hunter’s stroke. Neurosurgery 23:228-232, 1988
- Mapstone T, Spetzler RF: Vertebrobasilar insufficiency secondary to vertebral artery occlusion from a fibrous band. Case report. J Neurosurg 56:581-583, 1982
- Matsuyama T, Moriomoto T, Sakaki T: Comparison of C1-2 posterior fusion and decompression of the vertebral artery in the treatment of bow hunter’s stroke. J Neurosurg 86:619-623, 1997
- Okawara S, Nibbelink D: Vertebral artery occlusion following hyperextension and rotation of the head. Stroke 5:640-642, 1974
- Pamphlett R, Raisanen J, Kum-Jew S: Vertebral artery compression resulting from head movement: A possible cause of the sudden infant death syndrome. Pediatrics 103:460-468, 1999
- Powers SR, Jr., Drislane TM, Nevins S: Intermittent vertebral artery decompression: A new syndrome. Surgery 49:257-264, 1961
- Pratt-Thomas HR, Berger KE: Cerebellar and spinal injuries after chiropractic manipulation. JAMA 133:600-603, 1947
- Sheehan S, Bauer RB, Meyer JS: Vertebral artery compression in cervical spondylosis. Arteriographic demonstration during life of vertebral artery insufficiency due to rotation and extension of the neck. Neurology 10:968-986, 1960
- Shimizu T, Waga S, Kojima T, et al: Decompression of the vertebral artery for bow-hunter’s stroke. Case report. J Neurosurg 69:127-131, 1988
- Sorensen BF: Bow hunter’s stroke. Neurosurgery 2:259-261, 1978
- Tatlow WFT, Bammer HG: Syndrome of vertebral artery compression. Neurology 7:331-340, 1957
- Toole JF, Tucker SH: Influence of head position upon cerebral circulation. Studies on blood flow in cadavers. Arch Neurol 2:616-623, 1960
- Yang PJ, Latack JT, Gabrielsen TO, et al: Rotational vertebral artery occlusion at C1-C2. AJNR 6:98-100, 1985
