Spontaneous Deep Cerebral Venous Thrombosis
Authors
G. Michael Lemole, Jr., MD
Jeffrey S. Henn, MD
Mark Gerber, MD
Cargill H. Alleyne, Jr., MD*
Cameron G. McDougall, MD
Division of Neurological Surgery, Barrow Neurological Institute, St. Joseph’s Hospital and Medical Center, Phoenix, Arizona
*Current address: Department of Neurological Surgery, University of Rochester Medical Center, Rochester, New York
A 16-year-old female 2 weeks postpartum presented to the emergency room with a decreased level of consciousness. Her pregnancy had been complicated by late pre-eclampsia and a 3-day labor that eventually required cesarean section. Immediately postpartum, the patient was treated for endometritis and superficial phlebitis of the arm. She was discharged home 1 week later. From that time, she complained of progressively severe headaches associated with nausea and vomiting. She had no history of clotting dysfunction or miscarriage.
On initial examination, the patient was extremely lethargic. She only opened her eyes to pain and moaned incomprehensibly. She could, however, follow simple commands with her extremities. She had 4-mm reactive pupils, and her gaze was conjugate. Her face was symmetric and her tongue was midline. Her gag response was positive. Complete blood count and coagulation studies were normal.
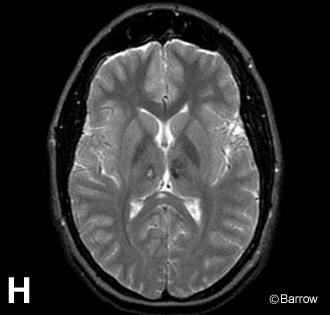
Imaging studies, including computed tomography (Panel A), demonstrated bilateral thalamic hypodensities. T2-weighted magnetic resonance (MR) imaging showed edema in this region, and diffusion-weighted MR imaging suggested infarction (Panel B). Axial (Panel C), coronal (Panel D), and sagittal (Panel E) MR venograms showed an absence of blood flow in the deep Galenic system and left transverse sinus. Follow-up MR images obtained several days later confirmed these findings. On T2-weighted MR imaging, areas of low-signal intensity associated with the internal cerebral veins, vein of Galen, and straight sinus suggested flow voids (Panel F). On T1-weighted MR imaging, however, the hyperintense signal thought to represent methemoglobin within these vessels indicated acute thrombosis (Panel G).
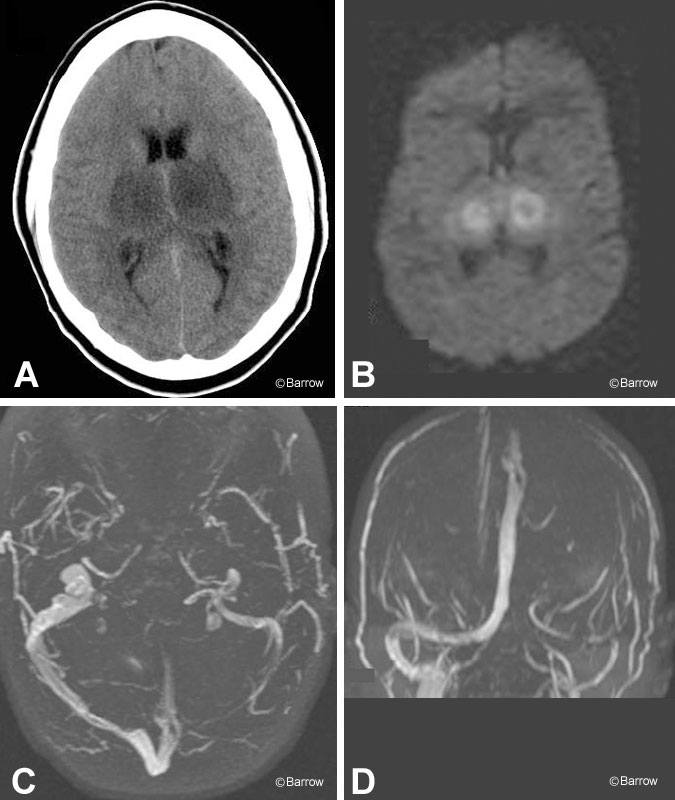
The patient was treated with intravenous anticoagulation therapy and gradually improved. At discharge to rehabilitation, she was awake and alert although disoriented. She had no obvious focal motor weakness but required assistance with ambulation due to truncal and gait ataxia. Long-term follow-up MR imaging showed resolution of the deep diencephalic edema with only slight evidence of permanent structural damage (Panel H).
Spontaneous venous thrombosis and infarction are rare but well-described complications of pregnancy. This patient’s imaging studies exquisitely demonstrate the venous and cerebral anatomy affected by spontaneous thrombosis of the Galenic system. The patient’s neurologic course strongly correlated with the site of thrombosis.