
Marked Improvement in Essential Hypertension After Surgical Obliteration of a Tentorial Dural Arteriovenous Fistula
Vivek R. Deshmukh, MD
Felipe C. Albuquerque, MD
Cameron McDougall, MD
Robert F. Spetzler, MD
Division of Neurological Surgery, Barrow Neurological Institute, St. Joseph’s Hospital and Medical Center, Phoenix, Arizona
Vascular compression of the medulla is a possible etiological factor underlying essential hypertension. We report a patient whose medically refractory essential hypertension improved significantly after microsurgical treatment of a tentorial dural AVF. A 37-year-old woman had a 5-year history of essential hypertension refractory to multiple antihypertensive medications. She reached neurosurgical attention when she developed intermittent hand and upper extremity numbness and facial weakness. MR imaging showed extensive subcortical white matter disease. Angiography revealed a tentorial dural AVF with retrograde leptomeningeal venous drainage. Endovascular obliteration of the fistula was unsuccessful because transvenous access was lacking and the arterial feeders were tortuous. She underwent a supracerebellar-infratentorial craniotomy for ligation of the fistula and suffered no complications. She remained normotensive and free from all antihypertensive medications for one year and now continues to have excellent control of blood pressure on a low-dose diuretic agent. This is the first reported case of significant improvement in medically intractable essential hypertension after ligation of a dural AVF. The patient’s systemic hypertension may have been the result of brainstem ischemia related to venous hypertension. The ischemia was alleviated by interrupting the fistula and reversing the venous hypertension.
Key Words: dural arteriovenous fistula, essential hypertension, neurogenic hypertension, venous ischemia
Abbreviations used: AVF, arteriovenous fistula; MR, magnetic resonance
Hypertension afflicts about 690 million people worldwide.17 It is the major risk factor for heart disease and stroke, two leading causes of morbidity and mortality in the United States.[32] Essential hypertension (hypertension without a known cause) constitutes 90 to 95% of all hypertensive patients.[29] Vascular compression of the left ventrolateral medulla has been proposed as an etiologic factor, and considerable scientific and anecdotal evidence supports the contention.[6,12,15,22,23,30,35] In such cases, microvascular decompression is an effective treatment of essential hypertension. [7,8,12,16,18] We report the first case of a patient with medically intractable essential hypertension who improved significantly after undergoing microsurgical obliteration of a tentorial dural AVF.
Case Report
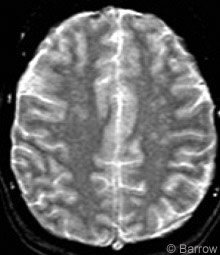
A 37-year-old woman had experienced intermittent left facial droop, left arm numbness, and bilateral hand numbness for 3 months. She also had a 5-year history of progressively worsening headaches. T2-weighted MR imaging (Fig. 1) demonstrated extensive changes in the subcortical white matter. These changes were more pronounced compared to earlier MR studies. Cerebrospinal fluid studies obtained to evaluate for multiple sclerosis were negative.
The patient had a 5-year history of hypertension. Extensive endocrinological studies, renal artery angiography, and abdominal ultrasonography to evaluate for pheochromocytoma were negative. Echocardiography showed early left ventricular hypertrophy. Along with the subcortical white matter changes, this finding was surprising given her age, and it was attributed to her refractory hypertension.
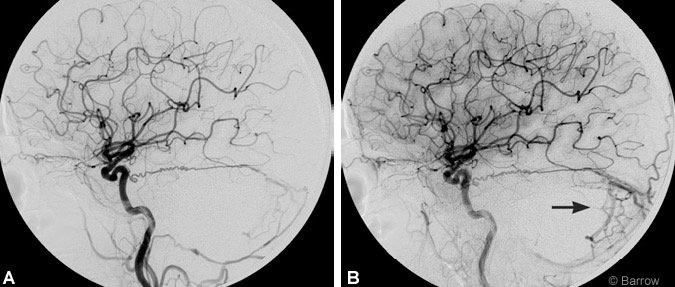
Cerebral angiography performed to rule out an underlying vasculitic process showed a tentorial dural AVF fed by a large Bernasconi-Cassinari artery, the ascending pharyngeal artery, and a transmastoid posterior meningeal artery branch from the external carotid artery (Fig. 2A). Drainage was primarily through a large tentorial vein that emptied into the transverse sinus and multiple cerebellar cortical veins (Fig. 2B).
When the patient was evaluated by the neurovascular service, she had no neurological deficits. The decision was made to attempt to obliterate the fistula through endovascular techniques. Transvenous embolization was not possible because of the location of the fistula and occlusion of the ipsilateral transverse sinus. Attempts were made to navigate to the fistulous point transarterially via the ascending pharyngeal artery. However, the tortuosity of the anastomotic connection between the feeders prevented access to the fistulous connection. At this point the decision was made to treat the lesion microsurgically.
In the neurosurgical operating suite the patient was placed prone, and a suboccipital craniotomy and supracerebellar-infratentorial approach to the tentorial fistula were performed. A prominent occipital sinus was ligated with vascular clips. With the use of the operating microscope, the fistulous pouch, which was identified at the inferior aspect of the tentorium along the midline, was cauterized with bipolar coagulation and divided sharply. The arterialized draining veins immediately turned the color of venous blood. Somatosensory evoked potentials remained unchanged throughout the case, and there were no intraoperative complications.
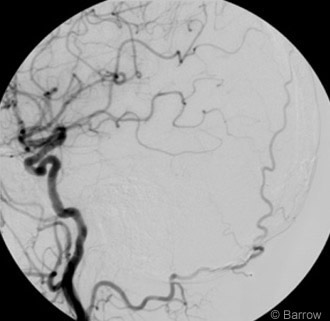
Postoperative angiography confirmed complete obliteration of the fistula (Fig. 3). The patient’s hospital course was unremarkable, and she was discharged on postoperative Day 4. She remained neurologically intact and suffered no complications as a result of treatment.
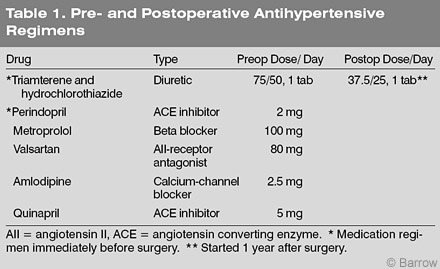
She was seen in clinic for follow-up 1 month, 2 months, and 1 year after surgery. The patient’s intermittent facial weakness and arm numbness resolved. She continues to have episodes of bilateral hand numbness. Her headaches improved mildly but persisted. Remarkably, her refractory hypertension resolved completely, and her blood pressure remained normal for 1 year. Then two blood pressure readings fell within the prehypertensive range (systolic blood pressure, 130-139 mm Hg; diastolic blood pressure, 80-90 mm Hg). She was placed on a low-dose diuretic, which has controlled her blood pressure (Table 1). Mean pre- and postoperative blood pressure values were 140.3/ 88.7 and 122.2/79.0 mm Hg, respectively. One-year follow-up angiography showed no residual or recurrent fistula. A 2-year postoperative MRI showed no further changes in subcortical white matter, reflective of improved blood pressure control.
She described no change in level of exercise or diet (salt intake) before or after surgery, and her weight has remained stable. She has been compliant with her medications since their initiation 4 years ago. She has no history of tobacco use. Upon extensive review of the patient’s history with her primary care physician, no other factor could be identified to explain the improvement in her blood pressure. The dramatic temporal relationship to the surgery implicates the fistula as the etiologic factor.
Discussion
Compression of the rostral ventrolateral medulla is a widely recognized neurogenic cause of essential hypertension. This concept was first popularized by Jannetta and coworkers,[11,12] and clinical studies in its support have been published.[6,15,22,23,30,35] Anatomic and physiologic studies have identified the left rostral ventrolateral medulla as the cardiovascular control center and have shown that pulsatile compression of this region can cause essential hypertension. [5,19,20,22,24,28] The use of MR imaging and MR angiography as screening tools has not yielded similarly compelling results, and the literature regarding the utility of MR imaging in this scenario is conflicting.[1,3,23,31] However, surgical decompression significantly alleviates hypertension in select patients.[7,8,12,16,18]
Other compressive causes of neurogenic hypertension include basilar impression and foramen magnum meningiomas. Dickinson et al.[4] described a patient with basilar impression who was hypertensive for 7 years before surgery. She remained normotensive for 2 years after a transoral odontoidectomy. Wörner et al.33 described a patient whose systemic hypertension improved after resection of a foramen magnum meningioma that had been compressing the left ventrolateral medulla (follow up, 14 months). These reports further validate the compressive theory of neurogenic hypertension.
Our patient represents the first report of surgical obliteration of a posterior fossa dural AVF that significantly alleviated essential hypertension. We postulate that venous ischemia caused essential hypertension in our patient for the following reasons. The pathophysiology of dural AVFs has been examined extensively, and venous hypertension plays a major, if not primary, role in the development of the symptoms and signs. High-risk dural AVFs have retrograde leptomeningeal venous drainage. These veins become arterialized by the high blood flow. The region of the posterior fossa drained by these veins experiences venous hypertension with resultant venous ischemia from inadequate drainage of poorly oxygenated blood. Transient ischemic attacks can occur in the drainage distribution.[2,10,14,27]
Several examples of this phenomenon have been described in the literature. Greenough and associates[9] reported a patient with a posterior fossa dural AVF that caused reversible, bithalamic hyperintensities, abulia, and memory difficulties. Ricolfi et al.[26] and Perkash et al.[25] reported patients with a posterior fossa dural AVF that caused reversible spinal cord edema and progressive myelopathy. In the Japanese literature, Nakai et al.[21] and Yamakami et al.[34] described reversible dementia and reversible diffuse white matter changes in patients with dural AVFs. Kawaguchi and associates[13] noted that regional cerebral blood flow, as shown by single photon emission computed tomography, improved after ligation of an anterior cranial fossa dural AVF. They also proposed a classification scheme for venous ischemia that depended on the presence of hyperintensity, enhancement, and hemorrhage.
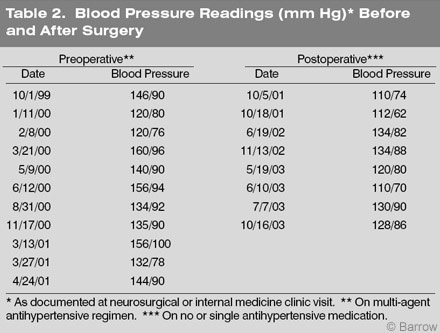
Our patient presented with intermittent weakness involving the face and arm and numbness involving the hands. These symptoms probably reflected brainstem ischemia from inadequate venous drainage. Her labile hypertension also may have been the result of intermittent ischemia in the region of the left rostral ventrolateral medulla. As evidence of this lability, two preoperative blood pressure readings separated by about a month were 120/76 and 160/96 mm Hg. Broad fluctuations in the systolic and diastolic blood pressure were common preoperatively (Table 2). Obliteration of the fistulous connection allowed the retrograde venous drainage to be interrupted and normal collateral venous drainage to be established. The venous ischemia then resolved. This report introduces the concept of brainstem ischemia caused by dural AVF as a surgically treatable cause of neurogenic hypertension.
Conclusion
Pulsatile vascular compression of the left rostral ventrolateral medulla causing systemic hypertension is a well-described phenomenon. This case demonstrates that tentorial dural AVFs may present with labile essential hypertension. The pathophysiology is likely related to venous hypertension and ischemia of the medulla. Posterior fossa dural AVFs should be included as a potential cause of surgically treatable neurogenic hypertension.
