Comprehensive Program of External Cuing to Enhance Procedural Memory in a Patient with Dense Amnesia*
Susan K. Kime, OTR†
David G. Lamb, PhD†
Barbara A. Wilson, PhD‡
†Division of Neurology, Barrow Neurological Institute, St. Joseph’s Hospital and Medical Center, Phoenix, Arizona
‡MRC Applied Psychology Unit, Cambridge, England
Abstract
This case study describes rehabilitation efforts with a 24-year-old woman who exhibited dense amnesia secondary to status epilepticus following a motor vehicle accident. She was 20 months postinjury upon entry into our day treatment program. The functional severity of her amnesia was reflected in numerous ways, including no recall of what she wore from day to day and an inability to find the toilet after 2 weeks in the program. A multidisciplinary comprehensive program of external cuing was established to exploit her preserved procedural memory. Objective measures of functional compliance were gathered over time and contrasted with both standard neuropsychological test scores and early levels of functioning in rehabilitation. Results demonstrated enhanced functioning via utilization of procedural memory. In addition, the patient actually demonstrated increased independent generalization of strategies and techniques over time. Practical treatment implications are reviewed and discussed.
Key Words : cuing, dense amnesia, neuropsychology, rehabilitation
Difficulty with memory is one of the most common cognitive deficits experienced after a brain injury.2,12 Such problems typically limit the afflicted person’s capacity for functional independence.13 A number of compensatory strategies have been tried with amnestic patients, including memory books,13 behavioral prosthetics such as watch alarms,1 and handheld microcomputers.3 At best, results of these intervention efforts have been moderately successful within narrowly defined circumstances.
In their review of the research in this area, Franzen and Haut1 found very limited generalization of these compensations to environments outside rehabilitation. In another review, Godfrey and Knight4 concluded that the gains obtained during active rehabilitation efforts were rarely maintained over time. Jennett and Lincoln7 argue that teaching memory compensation strategies “. . . is time consuming and the benefits are minimal compared with the effort,” and they note that “clinical psychologists and other therapists working in memory therapy are expensive.”(p 83) In contrast, Wilson15 found evidence of increased use of memory aids and compensations by patients 5 to 10 years after a cerebral insult. She hypothesized that the relevance of these strategies became more evident to the patients after discharge from rehabilitation “. . . as they were confronted by problems associated with the actuality of daily living.”15 (p 131)
External memory aids seem to be successful only to the extent that the patient’s procedural memory is intact and functional. The distinction of procedural memory from other types of memory has been described elsewhere,6,14 as has its potential to assist in the rehabilitation of memory deficits.5,8 In short, procedural memory involves the ability to recall how to do something, while declarative memory requires a person to recall specific facts or experiences. The case presented here offers a classic example of the difference between these two types of memory and presents evidence for the successful use of a patient’s intact procedural memory to dramatically improve her ability to function independently.
Illustrative Case
A 24-year-old woman suffered multiple orthopedic injuries in a motor vehicle accident on May 27, 1991. In August 1991, she developed status epilepticus while in the hospital. Her functional capacities were compromised, as evidenced by her requiring assistance for clothing selection, needing cues to perform personal hygiene tasks, and requiring direct supervision to assure compliance with her medication regime. She entered the Adult Day Hospital for Neurological Rehabilitation (ADHNR) on January 25, 1993 with the goal of improving her ability to complete selfcare and homemanagement tasks independently.
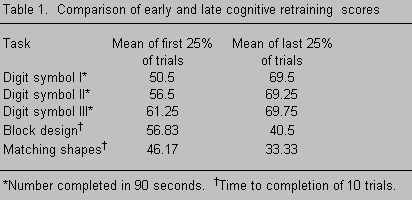
Upon admission, neuropsychological testing demonstrated that her performance on immediate recall of narrative passages and simple designs was borderline. With delays, scores on these tasks fell to the first percentile. Likewise, her ability to learn a list of 16 words was severely impaired: long-delayed recognition as well as short- and long-delayed free and cued recall were all five standard deviations below the mean. Her dense amnesia was clearly demonstrated during the first several weeks of the program. She was unable to remember where the toilets were located, the names of various therapists, the purposes of different sessions, or having participated in program activities from day to day.
Treatment
The treatment orientation at the ADHNR is somewhat unusual in its multidisciplinary, milieu approach and has been described in detail elsewhere.9,11 In short, there is considerable communication between all disciplines due to frequent staff meetings (four weekly) and a commitment to team development of individual treatment strategies. Also, admission to the ADHNR program requires active participation by the patient’s family during the course of rehabilitation. Finally, schedules at the ADHNR are consistent from week to week, providing maximum structure during the initial phase of treatment.
Numerous treatment strategies were employed to assist with the patient’s dense amnesia. When she initially arrived on the unit, she experienced considerable difficulty recalling the names of both staff and other patients. Both the patient and her family reported that recalling names had been problematic since her injury. Using a technique described by Wilson,16 she developed mnemonic cues to be associated with Polaroid photographs of staff and patients. For example, she linked the physical therapist with her job (“Heather is healthy”), related the neuropsychology fellow’s name with her brother (“Dave, like my brother”), and sometimes simply rhymed the names (“Dennis playing tennis,” “Janet on a planet”). Each cue was written on an index card that included her own associated drawing. The patient practiced linking the cues with the pictures every night and was tested by staff daily, with three trials in each session. Within 4 weeks, she was achieving approximately 90% accuracy rate on naming the pictures. The occupational therapist also had her practice naming staff and patients during various group sessions. Incredibly, 2 months after beginning this intervention, she reported independently using this technique to learn the name of one of her new neighbors.
In an extension of the photographic cuing technique, the patient and her family were asked to collect various photographs to mark events she had participated in since her accident. These photographs were assembled in an album and appropriately labeled for later reference. While in the program, she took pictures during community outings and added them to the photo album. In a personal communication almost 2 years after her discharge, she reported that she still adds photographs to the album and labels them. When asked why she continued this activity, she said “it gives me a time-frame,” indicating the value of this technique in placing amnestic persons within the context of a personal past.
The other primary treatment strategy involved the purchase of a datebooka and a watch alarm that chimed hourly as a reminder to refer to the datebook. Her datebook was broken into sections, including a daily time-log, instructions for using her watch, where to meet her therapist, each therapist’s name, and maps of the ADHNR and her apartment complex. Each therapy session had its own section with a brief description of the purpose of the session and the therapist’s name. Later, additional sections were incorporated within the datebook. These included sections for people with whom she had talked, letters she had written, movies she had seen, and a general calendar for future entries.
Initially, the patient resisted using the watch chime. She also was embarrassed by having to carry her datebook in public. Nonetheless, she was prompted to use the watch alarm during various therapy sessions throughout the day and at home. Different therapists would provide her with assignments and messages to convey to other therapists as a way to learn the procedures associated with using the datebook. Written procedures also were developed for almost every multistep task she encountered during her day. Trial runs were necessary to ensure that the steps were described in sufficient detail for her to be able to complete them independently. These procedures also were implemented by staff during her volunteer work-trial experiences.
In addition to the datebook and watch chime, the patient used an eraser board with information for tracking self-care and home duties. Her family was trained to use various cuing techniques and demonstrated excellent follow-through in this regard. Intervention also included several home visits by the occupational therapist, focusing on successful transfer of program techniques to the home environment. Toward the end of her stay at ADHNR, she was asked to track her activities in a more global manner, using a monthly calendar to plan for such events as payment of insurance, conditioning her waterbed, issuance of paychecks, watering her plants, and checking her smoke detector.
Methods
Dependent variables for this study were selected to reflect whether the patient generalized the above intervention techniques to independent home living. They included (1) percentage of compliance with checking her datebook when cued by watch chime; (2) number of entries under the action record in her datebook; (3) number of cross references in her datebook; and (4) number of separate entries on her monthly calendar. More specifically, the first dependent variable required that she use an hourly watch alarm that cued her to check her datebook for any information entered. The percentage of her compliance with this task was computed daily. At first, only those hours initialed by program staff or her mother were considered confirmed. After 33 days of using this procedure, however, the patient began to assume this responsibility herself. Second, in the action record of her datebook, she wrote notes to prompt herself to do specific tasks or to recall parts of a specific conversation. Third, she was encouraged to enter cross references to previous notes or entries to facilitate recall and follow-through. Finally, to assist with advance planning and to promote confirmation of completion of previous tasks, she made notes on separate monthly calendar pages.
These measures were taken at different times during the course of the patient’s recovery. Because she lived several hundred miles away from the hospital, follow-up data could not be collected during precise and consistent time periods. Therefore, all measures were averaged over the length of time they were collected and reflect the patient’s general performance during two periods while she was in the program and at three different follow-up periods. Specifically, the dependent variables represent mean performances during five distinct times: (1) the first 21 days after she began using her datebook during her ADHNR treatment, (2) the last 21 days before final discharge from the program, (3) approximately 4 months after discharge from the program (between 177 and 208 days after discharge), (4) approximately 7 months after discharge from the program (between 246 and 282 days after discharge), and (5) approximately 13 months after discharge from the program (between 443 and 460 days after discharge).
Results
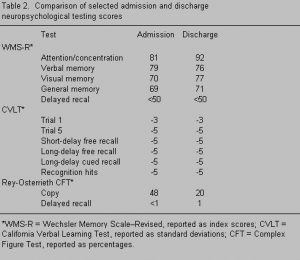 Results from multiple administrations of the Cambridge Behavioral Prospective Memory Test (CBPMT; Wilson and Evans, unpublished data) also documented improved procedural memory. The CBPMT requires the subject to perform a series of tasks during the testing period. At the start of the test, the subject is advised that she is free to use any means of remembering the tasks, including writing notes. When first administered the CBPMT, the patient’s total score was 40%. When retested 40 days later, her score improved to 80% and was 90% at the time of discharge. During the first administrations of the CBPMT, the patient took no notes. She took some notes part way into the second test, but they were incomplete and not referred to systematically in a timely fashion. By the last testing session, however, she began taking notes without any prompts and began checking her notes frequently to ensure completion of assigned tasks. That she spontaneously took notes with no recall of having been assessed before or any explicit knowledge of her previous performance demonstrates successful acquisition of procedural memory for both taking notes and checking them at a later time.
Results from multiple administrations of the Cambridge Behavioral Prospective Memory Test (CBPMT; Wilson and Evans, unpublished data) also documented improved procedural memory. The CBPMT requires the subject to perform a series of tasks during the testing period. At the start of the test, the subject is advised that she is free to use any means of remembering the tasks, including writing notes. When first administered the CBPMT, the patient’s total score was 40%. When retested 40 days later, her score improved to 80% and was 90% at the time of discharge. During the first administrations of the CBPMT, the patient took no notes. She took some notes part way into the second test, but they were incomplete and not referred to systematically in a timely fashion. By the last testing session, however, she began taking notes without any prompts and began checking her notes frequently to ensure completion of assigned tasks. That she spontaneously took notes with no recall of having been assessed before or any explicit knowledge of her previous performance demonstrates successful acquisition of procedural memory for both taking notes and checking them at a later time.
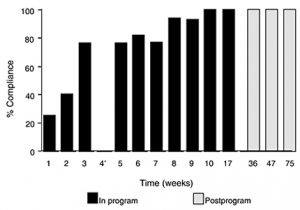
The patient’s compliance rate for checking the datebook when cued by the watch chime improved significantly (Fig. 1). Her compliance rate during the first 21 days of treatment was 47.6% with considerable cuing by both staff and family. After 64 days in the program, she independently produced 7 consecutive days of 100% compliance on this procedure. Her ability to continue independently at this rate at 4, 7, and 13 months after discharge attests to the stability of this procedural task over time. These results also substantiate the potential of this intervention strategy to generalize across a variety of settings and circumstances.
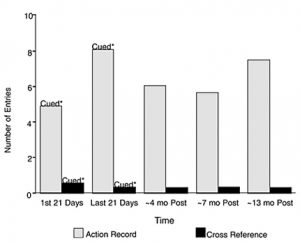
Figure 2 presents the patient’s action record and cross-reference utilization rates. Both the first and last 21-day periods represent rates that were achieved with significant cuing on the part of program staff and family. Her use of these strategies did not decline significantly once she left the program even though she received no cues from staff or family to enter such notes. Her performance is particularly impressive when observed 13 months after discharge.
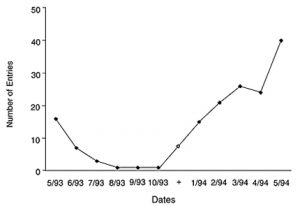
Finally, the use of the monthly calendar to track global activities and to assist with advanced planning was only introduced to the patient in the last 2 months of her rehabilitation (Fig. 3). Although the decline after leaving the program would be expected, the subsequent increase in use beginning 6 months after discharge is quite unexpected. Not only is the increase substantial, but it was achieved without the direct intervention of staff or family. This finding suggests the proliferation of a procedural compensation that was generalized from earlier, related strategies. Evidence of the longevity of this intervention is found in the occupational therapist having received a birthday card from the patient in each of the two years since her discharge from the program. The cards not only indicate the patient’s advance planning but her independent transfer of the information from year to year.
Discussion
Rehabilitation of a densely amnestic patient presents many obvious challenges. When attempting to take advantage of preserved procedural memory, a number of factors are critical for successful transition from a rehabilitation program to independent home living. First, a strong working alliance must be established with the family to provide continuity of intervention in the home environment. The working alliance with the family correlates significantly with the level of productivity after treatment.11 Intervention strategies must be organized and practiced daily by both staff and family. The coordination of efforts among multidisciplinary team members is also crucial in providing consistency with procedures and opportunities for practice in a variety of settings. Consistency is particularly important in the home environment, as suggested by Wilson.15 Even with such intense efforts, it required more than 2 months before our patient demonstrated a consistent 100% compliance in checking her datebook for entries. Successful generalization of these procedures to the home and work environments required additional time and effort from both staff and family.
The second major component of our patient’s rehabilitation involves the multidisciplinary milieu approach at ADHNR. The specific techniques were applied by different staff with various training backgrounds and treatment experiences. Despite these differences, however, the staff coordinated their efforts for maximum effect. For example, the patient complained of feeling as if she was in a dream and her life was not real. The neuropsychology fellow used individual psychotherapy sessions to work on this issue via discussions about awareness and acceptance of her deficits. At the same time, the occupational therapist tracked this problem during her memory training sessions by asking the patient if she still felt like she was in a dream. Initially, she always responded yes, life still felt dreamlike. With time, this feeling diminished and the patient attributed the improvement to having “pictures, a journal, and a datebook to look back at,” as well as “because I feel like I’m dealing with it more.” These quotes suggest that she responded positively to both the sense of continuity provided by the occupational therapist’s memory interventions (e.g., datebook, face recognition exercises) and the psychotherapy that focused upon increasing her awareness and acceptance. This case illustrates that if expectations are realistic and a rehabilitation program can provide the intense, comprehensive treatment necessary, external cues can be used to effectively facilitate functional enhancement of intact procedural memory.
*From: Use of a comprehensive program of external cuing to enhance procedural memory in a patient with dense amnesia. Brain Injury (in press). With permission of Taylor & Francis Publishing.
aThis datebook consisted of removable pages for each day, broken into three different areas: Appointments (from 7:00 a.m. to 8:00 p.m.), Action Record (a lined area for writing entries or reminders and taking general notes), and Summary (at the bottom of the page).
References
- Franzen MD, Haut MW: The psychological treatment of memory impairment: A review of empirical studies. Neuropsychol Rev 2:29-63, 1991
- Freeman MR, Mittenberg W, Dicowden M, et al: Executive and compensatory memory retraining in traumatic brain injury. Brain Inj 6:65-70, 1992
- Giles GM, Shore M: The effectiveness of an electronic memory aid for a memory-impaired adult of normal intelligence. Am J Occup Ther 43:409-411, 1988
- Godfrey HP, Knight RG: Interventions for amnesiacs: A review. Br J Clin Psychol 26:83-91, 1987
- Goldstein G, Ryan C, Turner SM, et al: Three methods of memory training for severely amnesiac patients. Behav Modif 9:357-374, 1985
- Graf P, Squire LR, Mandler G: The information that amnesic patients do not forget. J Exp Psychol Learn Mem Cogn 10:164-178, 1984
- Jennett SM, Lincoln NB: An evaluation of the effectiveness of group therapy for memory problems. Int Disabil Stud 13:83-86, 1991
- Kirn TF: Tapping into ‘procedural’ memory helps patients with amnesia to acquire new occupational skills [news]. JAMA 257:3187, 1987
- Klonoff PS, Lamb DG, Chiapello DA, et al: Cogni-tive retraining in a milieu-oriented rehabilitation program, in Maruish ME, Moses JA (eds): Theoretical Foundation of Clinical Neuropsychology for Clinical Practitioners. New Jersey, Lawrence Erlbaum: (In Press)
- Klonoff PS, O’Brien KP, Prigatano GP, et al: Cognitive retraining after traumatic brain injury and its role in facilitating awareness. J Head Trauma Rehab 4:37-45, 1989
- Prigatano GP, Klonoff PS, O’Brien KP, et al: Productivity after neuropsychologically oriented milieu rehabilitation. J Head Trauma Rehab 9:91-102, 1994
- Schacter DL, Rich SA, Stampp MS: Remediation of memory disorders: Experimental evaluation of the spaced-retrieval technique. J Clin Exp Neuropsychol 7:79-96, 1985
- Sohlberg MM, Mateer CA: Training use of compensatory memory books: A three stage behavioral approach. J Clin Exp Neuropsychol 11:871-891, 1989
- Squire LR: Memory and Brain. New York, Oxford University Press:1987
- Wilson BA: Long-term prognosis of patients with severe memory disorders. Neuropsychol Rehab 1:117-134, 1991
- Wilson BA: Memory therapy in practice, in Wilson BA, Moffat N (eds): Clinical Management of Memory Problems. San Diego: Singular Pub-lishing Group, pp 120-153:1992