Intrathecal Chemotherapy
Intrathecal Chemotherapy Overview
Intrathecal chemotherapy is a specialized treatment where chemotherapy drugs are directly injected into the cerebrospinal fluid (CSF). This fluid surrounds your brain and spinal cord. This method treats or prevents cancer in the brain and spinal cord area.
Cancer cells in the CSF can sometimes evade treatment because many chemotherapy drugs given by mouth or injected into a vein can’t cross into the CSF through the blood or through the brain itself. This natural protection system keeps harmful substances away from your brain. Intrathecal chemotherapy ensures the medicine can effectively reach and destroy these hidden cancer cells. Intrathecal chemotherapy can be administered via lumbar puncture or through a CSF reservoir-catheter system that is surgically placed under your scalp.
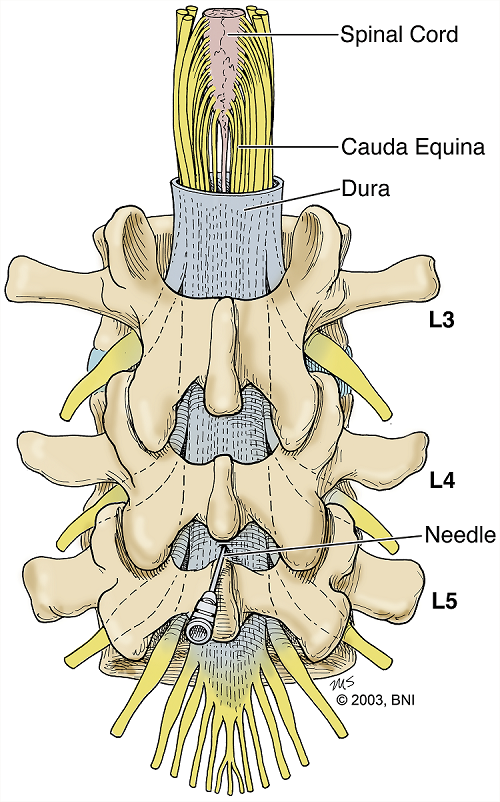
For a lumbar puncture (spinal tap), you’ll be asked to lie on your side with your knees pulled up to your chest, or you might sit and lean forward. Your doctor then injects the chemotherapy drug into the CSF through a small needle inserted in your lower back. While this may sound painful, you’ll receive medicine to numb the area and, if needed, medication to help you relax. The injection takes only a few minutes, though preparation and recovery time mean the entire process may take an hour or more. You might also need to lie flat for a few hours after the procedure to help prevent headaches.
An Ommaya reservoir is a CSF reservoir-catheter system which may be preferred for frequent intrathecal chemotherapy administration. This is a small dome-shaped device that is placed under your scalp by your neurosurgeon. The dome (CSF reservoir) has a tube that goes directly into a ventricle in your brain, allowing medications to be injected without requiring a needle in your back each time.
Intrathecal chemotherapy is a targeted approach to treating cancer in the brain and spinal cord, offering a way to reach areas that other forms of chemotherapy might not. If your doctor recommends this treatment, they believe it’s the best option to target the cancer effectively while minimizing exposure to the rest of your body. Side effects of intrathecal chemotherapy can vary depending on the drug used but may include headache, nausea, vomiting, and fever. These are usually temporary.

What is intrathecal chemotherapy used to treat?
Intrathecal chemotherapy may be used to treat cancers that affect the brain and spinal cord or are at risk of spreading to the CSF. It may also be used to treat cancer that has already spread to CSF.
It’s particularly effective because it delivers chemotherapy drugs directly into the cerebrospinal fluid (CSF), bypassing the barriers between blood-brain, brain-CSF, and blood-CSF, which can prevent many drugs administered through other routes from reaching the CSF.
Intrathecal chemotherapy can be used for:
- Leukemia: For acute and chronic leukemias, leptomeningeal therapy is generally not the most important component except for the following:
- Acute lymphocytic leukemia and Burkitt’s lymphoma: Intrathecal chemo is often part of treatment protocol due to up to 30% chance of central nervous system (CNS) involvement.
- Acute myeloid leukemia and chronic lymphocytic leukemia: Rarely, these leukemias can involve spinal cord and leptomeningeal disease that may require intrathecal chemotherapy.
- Lymphoma: Both Hodgkin’s and non-Hodgkin’s lymphoma, as a therapeutic treatment when they spread to CSF or as a preventive treatment when there is a high risk of spreading to the CNS.
- Solid tumors: When cancer has spread from the originating organ to the CSF space and if your doctor feels addition of intrathecal treatment is beneficial.
This approach ensures that the medication can effectively target cancer cells in a region that is otherwise difficult to reach, offering a better chance of controlling the disease in these sensitive areas.
Am I a good candidate for intrathecal chemotherapy?
Determining whether you are a good candidate for intrathecal chemotherapy involves several factors, and it’s a decision that you should make with your healthcare team. They will consider the type of cancer you have, its stage, whether it has spread to the central nervous system, your overall health, and how you’ve responded to other treatments.
It’s essential to have a detailed discussion with your oncology team about your specific situation. They can provide the most accurate advice based on your medical history, the specifics of your cancer, and the latest treatment options available. Your healthcare team’s goal is to choose the treatment that offers the best outcome while considering your quality of life and preferences.
Common Questions
What is the success rate of intrathecal chemotherapy?
The success rate of intrathecal chemotherapy can vary widely depending on several factors, including the type of cancer being treated, the stage of the disease, the specific chemotherapy drugs used, and your overall health. Its effectiveness can also depend on whether it’s being used as a treatment for existing disease in the CSF or as a preventative measure.
What kinds of chemotherapy drugs are given intrathecally, and what are their side effects?
Intrathecal chemotherapy involves administering drugs directly into the CSF surrounding the brain and spinal cord. Not all drugs can be injected this way to CSF. An appropriate intrathecal drug will be carefully selected by your healthcare team depending on your condition.
Side Effects
The side effects of intrathecal chemotherapy can vary depending on the specific drug used, the dosage, and the person’s reaction. Common side effects include:
- Headache is a common side effect, especially shortly after the procedure. It can range from mild to severe.
- Nausea and vomiting are also common and may be accompanied by a loss of appetite.
- Some people may experience fever and chills as a reaction to the treatment.
- The procedure itself can cause discomfort, including stiffness or pain in the neck area.
- Feeling unusually tired or weak is a common side effect of many cancer treatments, including intrathecal chemotherapy.
- Some people may experience changes in mood, confusion, or difficulty concentrating.
- In rare cases, drugs administered intrathecally can cause nerve damage, leading to symptoms such as numbness, tingling, or even paralysis.
It’s vital for you to report any side effects to your healthcare team, as there are often ways to manage these symptoms and improve comfort during treatment. Monitoring and managing side effects are critical components of the overall treatment plan for people receiving intrathecal chemotherapy.
Information and Resources
NIH National Cancer Institute: Definition of Intrathecal Chemotherapy