Barrow ENT Patient Opens Up About Throat Cancer
Identifying as a “Fighter” Helps Patient Dana Garrett Emerge From the Other Side of Cancer
Every time he passes by the breakfast bar of his Phoenix home, 69-year-old Dana Garrett sees a portrait of himself with a lopsided head, untamed hair, and a protruding tongue. “It cracks me up,” he said.
The artist? His now 7-year-old granddaughter. Her studio? The Neuro-Intensive Care Unit at Barrow Neurological Institute.
Afraid to disturb her papa’s cocoon of wires and tubes, she sat across his hospital room and occasionally peered up at him as she drew. He had just undergone a complex surgery for throat cancer.
Suspended in a Search for Answers
It started with a lump. Dana first noticed it in early 2022, nestled underneath his left ear and below his jaw line. He remembered it every time he shaved his face but gave it little thought, noting his uneventful medical history aside from a skiing accident and a sparse family history of cancer. When the tumor grew to the size of an egg and caught the attention of a co-worker, however, Dana scheduled an appointment with his primary care doctor for mid-February 2022.
“He took one look at it, poked around, and said, ‘I don’t know what it is, but we’re going to get aggressive about finding out what it is,’” Dana recalled. The doctor ordered a computed tomography (CT) scan that same day and referred Dana to a cancer specialist.
Feeling that his first few appointments at the initial cancer center were unproductive, Dana sought a second opinion from a community ear, nose, and throat (ENT) specialist. “What you’re seeing on the outside is only about 20 percent of what I’m seeing on the inside,” the ENT doctor explained after examining Dana’s throat with an endoscope.
The doctor then phoned Griffin Santarelli, MD, an ENT specialist in the Department of ENT and Skull Base Surgery at Barrow. “Dr. Santarelli knows his stuff, and he’s top of his game. He’s where you want to be,” the semi-retired doctor explained to Dana, securing him an appointment at Barrow for later that week.
“Wow,” Dana thought. “After all these years, I’m going full circle back to Barrow.”
A Lasting Impression
Dana’s first experience with the Institute wasn’t as a patient; it was as an audio-visual specialist. The Michigander had moved to Phoenix for its warmth and sunshine and started an audio-visual contracting firm, which Barrow hired to equip the neurosurgery operating room with live broadcast capabilities. Although live surgery technology is commonplace in medical education now, it was a monumental project in the 1980s.
As part of the job, Dana had the opportunity to see the OR in action. When he observed a real-life brain surgery at Barrow, he was awestruck by the professionalism, expertise, and teamwork of everyone who’d scrubbed in.
“My biggest takeaway from that visit—and I remember it well—was that if I personally ever had to go through that kind of procedure, it must be done at Barrow,” Dana said.
Throat Cancer Diagnosis: Preparing to Fight
When Dana and his wife first met with Dr. Santarelli on April 22, 2022, the otolaryngologist calmed them with his clear knowledge, honest communication, and affable demeanor. Dr. Santarelli also scoped Dana’s throat and, concerned with what he saw, scheduled a biopsy for the following week. In the meantime, he assembled a multidisciplinary team for Dana’s case—an approach that is a cornerstone of the Head and Neck Cancer Program at Barrow.
Dana spoke with both the radiation oncologist and medical oncologist assigned to his case before returning to Dr. Santarelli’s office on May 15, 2022 for the biopsy results and treatment plan. Dr. Santarelli confirmed Dana had back-of-throat cancer, formally known as oropharyngeal cancer, and laid out the treatment options.
“I was in tears,” said Dana’s wife, Barbara Rodriguez, who was already serving as a caregiver for her mom. “I went through all of those stages: shock, denial, anger.”
One treatment option consisted of both chemotherapy and radiation. Although less invasive than surgically removing the tumor, this approach would exclude Dana from being a candidate for surgical resection afterward.
Dana’s team, who had discussed his throat cancer at their weekly case conference, recommended starting with surgery to remove as much of the aggressive tumor as possible. They anticipated a complex procedure of 14 to 20 hours, with Dr. Santarelli removing the tumor and with plastic surgeon Andrew Blount, MD, reconstructing Dana’s tongue using skin from Dana’s forearm. He would then patch the forearm with a skin graft from Dana’s leg.
“Always a realist, I offered a potential third option: We do nothing and see what happens,” Dana recalled. Dr. Santarelli met him with a stern look. The expression remains imprinted in Dana’s memory, along with the surgeon’s warning: Dana would likely be dead within six months from the tumor closing off his airway.
In fact, after Dana had part of the cancerous mass removed during the biopsy procedure, he found himself breathing easier. He hadn’t recognized the gradual eclipse of his throat by the tumor until a portion of it was gone. “You keep creeping your car forward just a little bit at time until you bump the wall and you go, oh, I’m there,” he explained.
Dana and Barbara agreed to tackle the throat cancer with surgery first, at which point Dr. Santarelli asked Dana if he was a fighter. The surgeon spoke candidly about the difficult journey ahead and explained that Dana would play a crucial role in achieving a positive outcome. Dana thought back to his contracting career—all of the bid wars and the long days spent in the trenches. He responded, “I’ve been a fighter all my life. I’m not going to stop now.”
Throat Cancer Surgery: Moving to the Front Lines
On July 18, 2022, the night before Dana’s surgery, he and Barbara checked into a hotel neighboring Barrow. They went out for a nice dinner, but their pre-surgery anxieties sapped their appetites.
The next morning, they arrived at the hospital around 5 a.m. and began the pre-operative process. “I remember them saying, ‘You’re going to smell the inside of a basketball,’ and then I fell asleep,” Dana said.
Barbara spent the day in the waiting room, occupying herself with work and receiving ongoing reassurance from the OR team that her husband was doing well. Still, she felt relieved when Dana came out of surgery several hours earlier than expected.
“The surgical team was magical,” Dana said. They skillfully stitched his tongue back together after removing the tumor, meaning he didn’t need the forearm flap or skin graft after all. He prefers the alternative: a slightly shorter tongue than before.
Waking up from surgery was disorienting, though. Already prone to claustrophobia and still coming around from the anesthesia, Dana felt alarmed to find tubes jutting out of his body (including a 10mm tracheostomy tube obstructing his speech) and medical equipment crowding his bed. After the initial panic, he resigned to going with the flow and communicating through writing.
“Visits from different team members were regular,” Dana remembered. “The nursing staff and assistants were exceptional in performing their duties, and compassionate enough to have a conversation and make sure the healing process was going as planned. I had speech therapists, agility experts, and plenty of pokes and prods.”
When the team removed Dana’s tracheostomy tube, they asked him to carefully try speaking and explained that he might not be able to do so immediately. To everyone’s surprise, he asked loud and clear, “What do you want me to say?”
Although Dana had many visitors (in addition to his portrait artist) during his weeklong hospital stay, he grew antsy to get out of bed and back to work. Before he could head home, though, he needed to prove that he could safely eat semi-solid food. Relieved to finally have a meal that didn’t come through a feeding tube, Dana finished every bit of his roast beef dinner and prepared for discharge.
Radiation: A ‘Yes’ for Preventative Care
Not only was Dana’s throat cancer surgery less complex than expected, but his recovery was smoother too. His main complaints were a short-lived earache and some still-lingering weakness in his shoulder, for which he underwent six weeks of physical therapy. He also had a tooth nipped during the surgical opening of his jaw, which was later repaired by an oral surgeon.
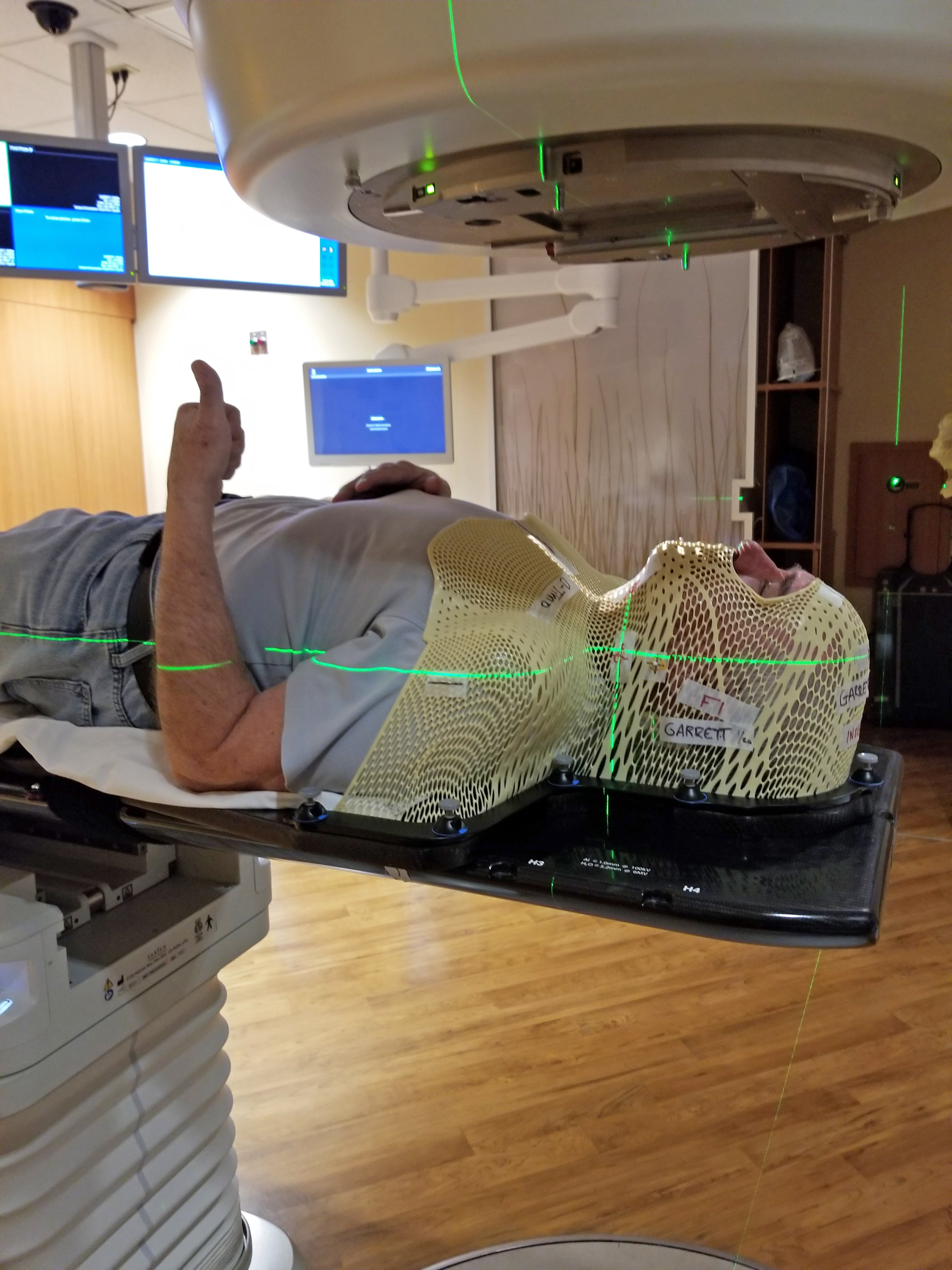
Dana began six weeks of low-dose radiation therapy in January 2023, even though his pathology report showed no signs of the tumor remaining. “They all agreed as a team that an ounce of prevention is worth a pound of cure,” Dana said, reiterating the aggressive nature of his type of cancer.
The claustrophobia struck again when Dana first donned the thermoplastic mask, which immobilizes the head and neck to ensure accurate delivery of the radiation beam. Music from the band “Chicago” and the compassion shown by the Department of Radiation Oncology staff helped soothe Dana during subsequent treatments, done five times per week for 10 minutes or less.
“Radiation therapy is one of the most effective, yet often one of the most difficult, treatments we use for patients with head and neck cancers,” said Dana’s radiation oncologist, William Kennedy, MD. “Although having state-of-the-art technology to provide the most precise radiation treatments available for my patients is important, what’s even more essential to me is having a well-trained, compassionate, close-knit team to help our patients every step of the way when they need us most. I’m proud of the people I have on my team that all play such a critical role in best caring for our patients; from the front office staff, to the therapists, dosimetrists, physicists, and nurses.”
As expected, radiation therapy became difficult for Dana about halfway through his treatment course. He developed side effects like fatigue, facial hair loss, and—the most distressing of all—a diminished sense of taste. “I think it was gradual, but one day I went, hey, I’m not tasting this salsa,” he remembered.
The loss of taste wrecked his appetite, so he subsisted on high-calorie nutritional drinks. Still, he lost about 50 pounds. Finally, after a nerve-wracking wait, his taste and appetite returned—albeit with a few changes.
“I always drank orange juice, and now citrus zings me,” he said. “And I was out with some friends who were in town, and I had this great big, gooey cinnamon roll; it set my mouth on fire.” But Dana views avoiding citrus and cinnamon as an acceptable trade-off for being cancer free. Fortunately, he can eat salsa—and taste it, too.
On his final day of radiation therapy, Dana rang the symbolic completion bell in front of a full house. His brother and sister-in-law were among the audience, having surprised him with a trip to Phoenix to celebrate the occasion. “That was really cool,” Dana said. “I took a minute to thank everybody for their kindness, and it was overwhelming. There’s a good camaraderie there. I know they deal with a lot of people who are anxious, and I was just very grateful.”
In This Together
Dana continues to visit Barrow for follow-ups, echoing Dr. Santarelli’s comment that they will be “best friends” for five years. But as his visits stretch farther apart, Dana’s (very organized) calendar is filling up with family time instead of doctors’ appointments.

In October, Dana and Barbara traveled to the Midwest to meet their first great-grandson, who was born a few months after Dana’s surgery. He calls the baby one of his three blessings since his throat cancer surgery, along with his two newest grandchildren. One of them shares a birthday with Dana’s discharge from the hospital. “I will not forget his birthday,” the devoted grandfather joked.
“Mr. Garrett’s ability to overcome his cancer is the outcome we wish for all patients,” Dr. Santarelli said. “The comprehensive head and neck oncology team at Barrow was able to provide him the tools to beat his cancer. It has been an awesome journey helping him through a difficult time so that he can enjoy doing the things he loves most, including hanging out with his grandchildren.”
Dana describes his family as teammates, who take turns stepping up for one another. It’s one reason why the team approach in the Head and Neck Cancer Program resonated deeply with him and Barbara.
“I feel honored to be here at Barrow,” he said. “You definitely feel part of a family; that they take a very strong interest in your case. Everyone’s treated with such respect.”
“I feel honored to be here at Barrow. You definitely feel part of a family; that they take a very strong interest in your case. Everyone’s treated with such respect.”
Dana Garrett, Barrow Patient
The feeling is mutual for the physicians. Reflecting on Dana’s outcome, medical oncologist Robert Yoo, DO, said, “It was a tremendous opportunity for me to work with our great ENT surgeons and radiation oncology as a multidisciplinary team to help Dana go through his journey to beat his throat cancer.”
Writing the Next Chapter
Dana’s beard is filling out, covering his already subtle scar. On May 5, he and Barbara will celebrate their 25th wedding anniversary. He still remembers her phone extension at the college where they both worked, the way he fumbled over his words when he tried to ask her on a first date, their long lunches at Durant’s steakhouse, and her marriage proposal at The Grapevine restaurant in Old Town Scottsdale.
As he navigated his demanding treatments, Dana found comfort in having Barbara by his side at nearly every appointment. Together, they debriefed each visit, jotted down questions, and made weighty decisions. He also described his strong faith in God and prayers from his church community as instrumental to his healing.
“His outcome is what we strive for as an institution,” Dr. Santarelli said. “Head and neck cancer is life changing and overwhelming. Providing the tools to confront, manage, and overcome your disease is something we pride ourselves on most at Barrow. Helping Mr. Garrett battle his cancer through surgery and radiation is what makes this the most rewarding job.”
Dana’s advice to other patients is to stay informed, but rein in the overthinking. While he believes it’s important to do your research and have honest conversations with your care team, he recommends taking things one day at a time.
As a care partner, Barbara felt grateful to have a sturdy safety net of family and friends to help her process her emotions. She encourages other care partners to lean on those who will graciously lend an ear while withholding judgment.
When it comes to the possibility of cancer recurrence, Barbara finds herself ruminating on the “what ifs.” But Dana has always helped her challenge those thoughts by focusing on the facts and on the present. For him, that possibility is “out of sight, out of mind.”
“We all know that none of us are getting out of this game alive,” Dana said. “At some point, my number’s coming up. I’m glad it’s not yet, but I’ll take that when it comes.”