Remyelination: Barrow Neuroimaging Scientists Explore ‘Next Frontier’ of MS Treatment
Neuroimaging scientists at Barrow Neurological Institute have received $875,000 in grants to further their research of remyelination. Boosting this natural repair process in the central nervous system is widely considered the “next frontier” of multiple sclerosis treatment.
The National Institutes of Health (NIH) has awarded an R21 grant to Ashley Stokes, PhD, an assistant professor in the Barrow Neuroimaging Innovation Center, to explore the role blood flow plays in the loss and spontaneous repair of myelin, a substance that insulates nerve fibers. In a complementary project funded by the National Multiple Sclerosis Society, associate professor Richard Dortch, PhD, aims to develop a widely accessible method for imaging myelin changes.
Their efforts to elucidate factors that contribute to myelin regeneration, identify therapeutic targets, and equip institutions with tools to evaluate remyelination therapies could help lay a foundation for future clinical trials.
What is Remyelination?
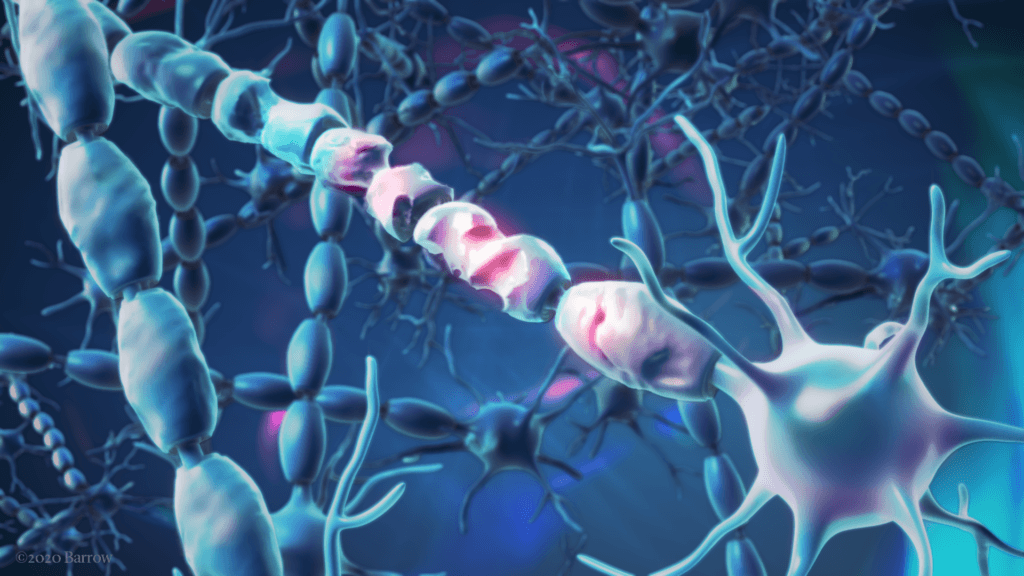
When nerve cells communicate with each other, they send electrical signals via axons. Similar to the way electrical wires are insulated by plastic or rubber, axons have a protective coating of fatty tissue. This membrane, known as myelin, not only shields the nerve fibers from damage but also facilitates the rapid transmission of electrical signals.
In multiple sclerosis (MS), the body’s immune system mistakenly targets the myelin sheath. These attacks leave inflammatory damage, evident on imaging scans as lesions. The destruction of this layer—known as demyelination—disrupts electrical impulses and, consequently, the bodily functions those impulses control.
MS affects every person differently. Some common symptoms include muscle spasms, walking difficulties, fatigue, vision loss, and problems with memory and thinking.
Sometimes, the body will restore myelin on its own—a phenomenon known as remyelination. This has been observed in patients with relapsing-remitting MS. This form is characterized by temporary episodes of symptoms followed by periods of recovery.
However, MS is variable and unpredictable—from its symptoms to the course it takes. Remyelination is no exception to this heterogeneity.
“Sometimes, lesions don’t remyelinate,” Dr. Stokes said. “Sometimes, they just continue to demyelinate. Then you have more axonal loss, which leads to more disability and symptoms.”
Even when myelin repair does occur, it is often incomplete. This leaves irreversible damage to axons in the brain and spinal cord, which accumulates over time with repeated attacks.
“Then sometimes people advance into more progressive forms of the disease, where there really is no break—just continuous disability,” Dr. Stokes said.
Scientists are trying to determine why remyelination is so inconsistent and whether therapies to promote this mechanism could improve long-term outcomes for people with MS.
Why Blood Flow?
Recent studies have suggested that the body’s ability to rebuild myelin depends on the volume of oxygen-rich blood delivered to nerve cells, known as perfusion. While altered perfusion has been reported in MS, the relationship between perfusion and myelin specifically has not been fully characterized in living subjects.
Additionally, current imaging biomarkers—biological characteristics that can be measured with imaging technology—show static levels of myelin but cannot predict changes.
Dr. Stokes’ project, supported for two years with a $275,000 R21 grant, aims to develop magnetic resonance imaging (MRI) biomarkers to determine whether blood vessel function can anticipate demyelination and remyelination of MS lesions. She will focus specifically on the relapsing-remitting form of the disease.
To capture changes in blood flow, Dr. Stokes will use spin- and gradient-echo (SAGE)—an advanced multi-contrast perfusion MRI method. She first applied this sequence to brain tumor research and then expanded it for use, without contrast agents, in Parkinson’s disease studies. To Dr. Stokes’ knowledge, no other institution is using SAGE for studying MS.
“The unique thing about this method is that we can look at total blood flow and volume, and then we can also look at the microvasculature specifically,” she said.
Dr. Stokes has previously used SAGE to probe perfusion changes in MS, thanks to a grant from Barrow Neurological Foundation. She collaborated with Dr. Borazanci to compare perfusion scans with self-reported quality-of-life measures in more than 50 patients.
“We didn’t see a relationship between perfusion changes and quality of life, unfortunately, and that’s probably related to heterogeneity in the MS population,” Dr. Stokes said.
However, that study would ultimately provide the data that Dr. Stokes needed to apply for the R21 grant.
Homing in on Myelin and Perfusion
After Dr. Dortch joined the Neuroimaging Innovation Center in the fall of 2019, he and Dr. Stokes began discussing a more specific project that would examine perfusion and myelin content in MS. He already had a special interest in myelin and had been developing an MRI method, known as selective inversion recovery (SIR), that can provide information on how much of the protective coating is still present within MS lesions.
“We had this idea that there would be a relationship between perfusion and myelin content, but we didn’t have the data,” Dr. Stokes said. “Previous investigators have shown that you can take a ratio of two clinical images and get a map that indirectly reflects myelin content. Using this method, we found a relationship between this indirect marker of myelin and our specific marker of microvascular perfusion.” These results were published last year in the Multiple Sclerosis Journal – Experimental, Translational and Clinical.
The R21 grant will enable Dr. Stokes and Dr. Dortch to pursue more specific data about the relationship between myelin and perfusion.
The researchers will work with Barrow MS neurologist Michael Robers, MD, to recruit participants for the study. Patients with active MS lesions will periodically undergo both a perfusion scan and myelin scan. Dr. Stokes will evaluate the relationship between myelin and perfusion longitudinally, by looking at myelin changes throughout each patient’s disease course, and cross-sectionally, by comparing the results in people with MS to people without the disease.
“I think one of the things that Barrow does really well is bring together the physicians with the scientists to answer some of these ‘next-frontier’ questions,” Dr. Stokes said. “Having this team of people with complementary expertise is critical. Dr. Robers brings clinical expertise in MS, and the link between perfusion and myelin combines my expertise with that of Dr. Dortch. This project started from the right combination of people and timing.”
Seeking the ‘Best of Both Worlds’ in Myelin Imaging
While Dr. Stokes aims to address the lack of specific biomarkers for predicting and tracking myelin loss and repair, Dr. Dortch hopes to overcome another obstacle in remyelination therapy development. This is the absence of established and easy-to-implement MRI measures of myelin repair.
“There are many different imaging methods that can look at demyelination and remyelination,” he said. “The challenge is that they require specialized approaches that aren’t available everywhere, and they’re challenging to interpret. In contrast, while conventional sequences are sensitive to this process, they’re not very specific because there are a lot of things going on simultaneously in MS.”
Dr. Dortch sees SIR as an ideal solution. This proposal has earned him a $600,000 grant from the National MS Society and aligns with the organization’s “Pathway to Cures” roadmap for MS research.
Dr. Dortch will be developing SIR sequences based on conventional MRI sequences that any hospital can acquire. This is known as a “turnkey” or “push button” imaging solution. In addition, automated software tools will be developed to analyze SIR data, removing the need for a physicist or an on-site clinical scientist to interpret the results.
“We’re trying to get the best of both worlds: something that’s easy to implement but also gives us improved specificity,” Dr. Dortch said.
Selective Inversion Recovery: Journey to Clinical Application
Dr. Dortch began developing SIR during his postdoctoral fellowship. At the time, researchers had only applied the technique to animals because it was relatively slow. After spending about a decade optimizing the approach, Dr. Dortch and his colleagues reduced the whole-brain imaging scan time from 30 minutes to six.
“We really started from fundamental development to translation and now clinical application,” he said. “That was the primary driving factor when I moved here a few years ago, the ability to make a real impact in patients and to get this into clinical care. Barrow is the ideal place to do that.”
With this grant, Dr. Dortch intends to establish methods that yield consistent SIR-related myelin measures across different MRI scanners. He will also test the ability of SIR to measure remyelination after relapses in individuals with relapsing-remitting MS. Ping Wang, PhD, an associate professor in the Neuroimaging Innovation Center, will assist with sequence development and data analysis.
In addition to being easy to implement and interpret, SIR may allow researchers to test emerging therapies with fewer subjects and for shorter durations by providing more consistent, sensitive, and specific measures than those currently available.
This project represents the goal of the North American Imaging in MS (NAIMS) Cooperative, which Barrow joined last summer after an application process. Through this network, academic centers across the United States and Canada share new imaging tools and work to standardize them for large-scale clinical trials.
“This puts us in a position to really, once this method is developed with this grant, have this network of sites that are ready to use it,” Dr. Dortch said.