Hemorrhagic Stroke
Overview
A hemorrhagic stroke is when a blood vessel leaks or bursts in the brain. This bleeding in the brain—known as a brain hemorrhage—then puts pressure on surrounding brain cells, which causes damage to brain tissue.
There are three kinds of hemorrhagic stroke:
- Intracerebral Hemorrhage: This type of hemorrhagic stroke happens when a blood vessel bleeds or ruptures, leaking blood into the surrounding brain tissue within the brain.
- Subarachnoid Hemorrhage: This type of hemorrhagic stroke occurs when a blood vessel on or near the surface of the brain ruptures and causes bleeding into the space between the brain and the tissues covering it.
- Intraventricular Hemorrhage: This describes a hemorrhagic stroke that causes bleeding into the open spaces in the brain that contain cerebrospinal fluid (CSF). It is much less common than intracerebral and subarachnoid hemorrhages.
When to call 9-1-1: Any kind of hemorrhagic stroke is life-threatening and warrants immediate medical attention. If you or someone around you experience the sudden onset of a ‘thunderclap headache’ (often described as the worst headache of your life), paralysis of the face or other body parts, nausea and vomiting, or light sensitivity (photophobia), call 9-1-1 and wait for help to arrive.
What causes hemorrhagic stroke?
Hemorrhagic strokes are generally caused by conditions that weaken blood vessel walls. High blood pressure–also known as hypertension—or a ruptured aneurysm or arteriovenous malformation (AVM) are the most common causes. A genetic disorder called hereditary hemorrhagic telangiectasia (HHT) can also lead to hemorrhagic stroke because it causes multiple AVMs to form, potentially resulting in bleeding from the tangles of blood vessels.
Other conditions that can increase risk include trauma or head injury or overuse of blood-thinning medications like warfarin or aspirin.
There’s also a high risk of hemorrhagic stroke following an ischemic stroke, or a stroke caused by a blocked artery. This is called a hemorrhagic conversion, and the risk of hemorrhagic stroke increases dramatically in the days (up to two weeks) after a large ischemic stroke.
In addition to these causes, modifiable and non-modifiable risk factors can increase your likelihood of a stroke. Modifiable risk factors, or risk factors that you can influence or change, include:
- Uncontrolled high blood pressure
- Diabetes
- High cholesterol
- Poor diet, particularly one high in salt, sugar, and saturated fats
- Obesity and a sedentary lifestyle
- Smoking and excessive alcohol use
- Use of cocaine or other illegal drugs
- Head trauma
- Infection
Factors that you cannot influence or change, called non-modifiable risk factors, include:
- Your age and gender: The risk of stroke increases with age, and women are at a slightly higher lifetime risk of stroke than men. What’s more, women are also more likely to experience a brain hemorrhage.
- Your genetic predispositions: A family history of stroke or vascular disease affects stroke likelihood.
- Your race: People of African American or Hispanic descent have a higher stroke risk, in part due to higher rates of hypertension and diabetes.
That said, regular check-ups with your healthcare provider to recognize and then manage these risk factors can significantly reduce your stroke risk.

Hemorrhagic Stroke Symptoms
The signs of a hemorrhagic stroke depend on three things: the side of the brain affected, the part of the brain affected, and how severely the brain is injured.
These three variables mean a hemorrhagic stroke can present in several ways. The hallmark sign is a thunderclap headache—a sudden headache often described as the worst headache pain a person has ever felt. Sensitivity to light usually accompanies this type of headache.
Symptoms of a hemorrhagic stroke may come on suddenly or develop over a handful of days. You or someone you know might experience:
- Deficits in your vision, blurred vision, or blindness in one or both eyes
- Pain above and behind the eye
- Facial droop
- Loss of ability to understand or express speech
- Partial or total loss of consciousness
- Sudden numbness or weakness of the face, arm, or leg, most noticeably on one side
- Stiff neck
- Seizure
- Sudden vertigo, an off-balance or spinning sensation
- Vomiting or severe nausea
- Urinary incontinence
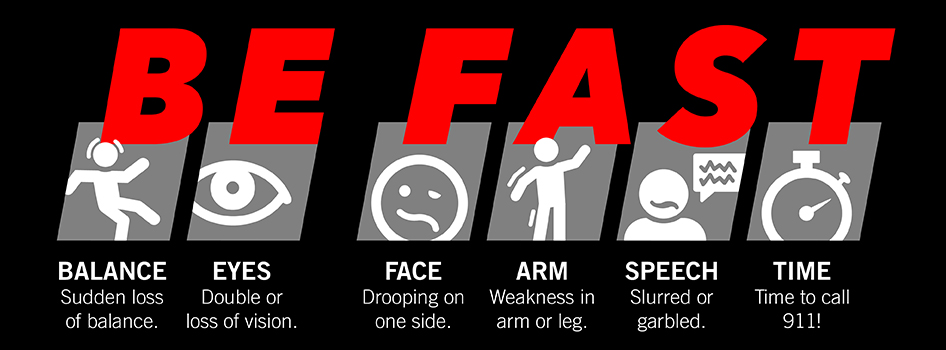
Quickly recognizing a stroke and calling 9-1-1 leads to a faster diagnosis and treatment and a better recovery. Here’s how you can BE FAST when it comes to a stroke:
- B – BALANCE: Ask the person to walk. Do they have trouble keeping their balance or walking normally?
- E – EYES: Ask the person about their eyesight. Have they lost vision or experienced vision changes in one or both eyes?
- F – FACE: Ask the person to smile. Does one side of the face droop?
- A – ARMS: Ask the person to raise both arms. Does one arm drift downward?
- S – SPEECH: Ask the person to repeat a simple phrase. Is their speech slurred or strange?
- T – TIME: If you observe any of these signs, call 9-1-1 immediately.
Hemorrhagic Stroke Diagnosis
Determining whether a stroke is hemorrhagic or ischemic as soon as possible is critical, as the treatment is different for each type of stroke. Brain imaging should be done immediately upon arrival at the hospital or curbside in a mobile stroke unit if it’s available for a definitive diagnosis. Ideally, diagnosis happens within 60 minutes or less from when you first notice symptoms.
If you have symptoms of a stroke, your care team will perform several of the following to reach a diagnosis quickly:
- Physical and neurological exam: Your healthcare provider will ask about your symptoms, overall health, and family history of stroke or related conditions. Next, they’ll complete a neurological examination to assess your neurological function, including reflexes, coordination, strength, and sensation.
- Cerebral angiography: The gold standard for detecting vascular lesions, cerebral angiography uses a special dye and X-rays to take detailed images of the blood vessels in the brain. A thin tube is inserted into an artery, usually in the leg, and guided up to the brain to deliver the dye. This allows doctors to see issues like a burst blood vessel, aneurysm, or abnormal vessel formation. It’s invaluable in diagnosing the cause of a hemorrhagic stroke and planning the best treatment.
- Electrocardiogram (ECG): An electrocardiogram is a simple and timely test that records electrical signals in the heart and can detect irregular heart rhythms.
- Echocardiogram: Also known as an “echo,” an echocardiogram is a non-invasive imaging test that uses ultrasound waves to create detailed pictures of the heart and its structure, function, and movement.
- Cerebrovascular testing: This group of testing describes the various tools used to diagnose conditions affecting the blood vessels inside and around the brain.
- Blood tests: These include a complete blood count (CBC) to check for infection, clotting issues, or anemia; coagulation tests to assess blood clotting ability; glucose levels to rule out hypoglycemia; lipid panels to check cholesterol; and markers for infectious or clotting disorders.
- Lumbar puncture: Also known as a spinal tap, a lumbar puncture is not routinely used to diagnose a stroke but may be done in specific cases where additional information is needed to clarify the diagnosis—particularly when there’s suspicion of a subarachnoid hemorrhage or another condition mimicking stroke. A lumbar puncture involves a needle being inserted into the lower part of the spinal canal to collect cerebrospinal fluid (CSF) for analysis.
Ideally, an initial assessment is completed within 10 minutes. Within 25 minutes, an MRI or CT scan is done. And in 60 minutes or less, a diagnosis is made and treatment is initiated.
Our team at the Petznick Stroke Center can perform a full range of diagnostic tests to determine the exact cause of a stroke 24 hours a day, seven days a week.

Hemorrhagic Stroke Treatments
It’s crucial to treat hemorrhagic stroke quickly to save as much brain tissue as possible. If the appropriate care is received within the first four hours and 30 minutes of the onset of symptoms, the impact of a stroke can be minimized. The longer a stroke goes untreated, the more brain cells die and the more difficult recovery becomes.
The first phase of treatment focuses on stabilizing a person’s vital signs and stopping bleeding in the brain. Medications are given to reverse the effects of blood-thinning medicines. The responding medical team may also take steps to lower blood pressure, reduce swelling in the brain, reduce or prevent seizures, and avoid blood vessel spasms (vasospasm).
Surgical Treatments
- Endovascular surgery: This treatment is a minimally invasive surgical procedure that uses catheters and devices passed through arteries in the arm or leg to repair the weak spot or break in a blood vessel, like an aneurysm or ruptured arteriovenous malformation (AVM). The tube is then used to install a device to repair the damage and prevent further bleeding.
- Endovascular embolization: Also known as coiling, a catheter is used to place coils inside an aneurysm, promoting clotting and sealing off the weakened area of the blood vessel.
- Aneurysm clipping: In this procedure, a small clip is placed at the base of an aneurysm to isolate it from normal blood circulation, preventing it from rupturing or bleeding again if it bursts.
- Craniotomy for hematoma evacuation: During this procedure, neurosurgeons remove a portion of the skull—known as a craniotomy—to access and clear out pooled blood, called a hematoma, that compresses brain tissue. This, in turn, relieves the pressure caused by swelling or bleeding.
- Arteriovenous malformation (AVM) surgery: This is the removal or repair of an abnormal tangle of blood vessels in the brain that leads to high-pressure blood flow. In this process, surgery, embolization, or radiation therapy may be used to repair the abnormal blood vessels that caused the hemorrhage to prevent additional bleeding and ease complications.
Nonsurgical Treatments
- Blood pressure management: Since high blood pressure is the most common risk factor for stroke, medications to lower or stabilize blood pressure are often an essential part of treatment.
- Cholesterol-lowering drugs: Drugs like statins play a crucial role in managing stroke risk by lowering cholesterol levels and improving outcomes after a stroke.
- Anti-seizure medications: If a stroke causes seizures or there’s a high risk of them occurring, your doctor will prescribe anti-seizure medications.
- Blood sugar control: Maintaining optimal blood glucose levels with insulin or oral medications reduces the risk of stroke complications and further damage for those with diabetes.
- Antithrombotic reversal agents: If you’re taking blood thinners (antithrombotic medications such as apixaban or aspirin) and have a hemorrhagic stroke, doctors may give you reversal agents to quickly stop the blood-thinning effect. This helps reduce further bleeding in the brain and lowers the risk of complications.
Neuro-Rehabilitation for Quality of Life
Neuro-rehabilitation is key to stroke recovery. While it doesn’t reverse brain damage, neuro-rehabilitation can help stroke patients achieve the best long-term outcome possible.
Rehabilitation treatments will vary depending on the part of the brain affected and the severity of the stroke. They can be provided in an acute care hospital, a rehabilitation hospital, or an outpatient setting. At Barrow Neurological Institute, our CARF-accredited Neuro-Rehabilitation Center offers inpatient, outpatient, and transitional rehabilitation programs. We also lead the industry in using neuro-robotics. These cutting-edge technologies allow patients to reach unprecedented heights in function and independence.
Complications of a Hemorrhagic Stroke
Depending on the extent of brain damage after a hemorrhagic stroke, a range of neurological complications can occur. They can include:
- Muscle weakness or loss of movement: Strokes can cause paralysis on one side of the body or the loss of control of a particular set of muscles, like an arm or side of the face.
- Decreased sensations: In the parts of the body affected by stroke, pain or persistent numbness can occur.
- Cognitive challenges: Memory loss is common following hemorrhagic stroke, as well as difficulty thinking, reasoning, and understanding concepts.
- Difficulty talking or swallowing: A stroke can affect the muscles in the mouth and throat, making it hard to speak, swallow, or eat.
- Seizures: Abnormal bursts of electrical activity in the brain, known as seizures, can become more common after a stroke.
- Severe headaches: Changes in the brain after a stroke can affect the blood vessels in the brain, leading to headaches or episodic migraines.
- Loss of vision: Damage to the nerves controlling the eyes can lead to movement problems, which can cause the eyes to have trouble working together.
- Changes in behavior or ability: Stroke survivors can become withdrawn and may require more support with self-care tasks, like grooming.
- Onset of a mental health disorder: Depression and anxiety can follow a stroke, as well as general difficulty in coping with feelings and emotions in a healthy way.
Recognizing a stroke quickly and calling 9-1-1 leads to a faster diagnosis, treatment, and recovery. When it comes to any stroke, it’s critical to BE FAST.
Common Questions
How common is hemorrhagic stroke?
Nearly 800,000 people suffer a stroke every year, but only 13 percent of these strokes are hemorrhagic. Although they make up a smaller percentage of strokes, hemorrhagic strokes are responsible for 40 percent of all stroke deaths.
Who is likely to experience a hemorrhagic stroke?
Hemorrhagic strokes can happen at all ages, but surprisingly, they’re more likely to occur in young people. Hemorrhagic strokes account for nearly 50 percent of strokes in children.
Black Americans, Hispanic Americans, and Native Americans all have a higher risk of stroke than white Americans, and when it comes to hemorrhagic stroke, black Americans and Hispanic Americans have a higher risk of recurrence than white Americans.
Additionally, if you’ve had a stroke, you’re at high risk for experiencing another one: one in four stroke survivors has had another stroke within five years of the first one. Other risk factors include high blood pressure, high cholesterol, heart disease, diabetes, and sickle cell disease.
What is the prognosis for those with hemorrhagic stroke?
The odds of survival after hemorrhagic stroke depend on the severity of the stroke and how quickly a person has received treatment. Generally speaking, hemorrhagic strokes are more likely to be associated with long-term disabilities and higher mortality rates.
Recovery from a stroke is often a long, arduous process, and it’s estimated that between 12 to 39 percent of hemorrhagic stroke survivors can achieve long-term functional independence. Some deficits after a hemorrhagic stroke can be permanent, and assistive devices, such as communication aids or a wheelchair, may be required.
That said, consistent effort is essential: many patients will see the most progress within the first six months after their stroke. Starting rehabilitation and therapy as soon as possible helps to improve outcomes.
Can hemorrhagic stroke be prevented?
The good news is that most strokes are preventable. Approximately 80 percent of all strokes can be prevented by lifestyle and behavior modification and control of healthcare conditions like diabetes, obesity, and high cholesterol.
If you have any of the following risk factors, please speak with your trusted healthcare professional to come up with a plan to reduce your risk:
- High blood pressure, specifically systolic blood pressure greater than 140 mm/Hg and diastolic blood pressure greater than 85 mm/HG.
- Smoking
- Excessive alcohol consumption
- Physical inactivity and obesity
- Diabetes: Hemoglobin A1c needs to fall below 5.7 percent.
- Hypercholesterolemia, or high levels of “bad cholesterol” (LDL)
Resources
American Stroke Association: Hemorrhagic Stroke
National Institute of Neurological Disorders and Stroke (NINDS)