
Hypopituitarism
Overview
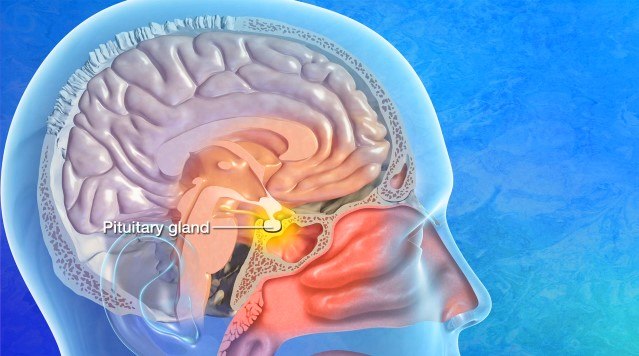
Hypopituitarism is when the pituitary gland doesn’t produce normal amounts of some or all of its hormones. When levels of one or more of these pituitary hormones are low, the body can be affected in many ways, including growth, blood pressure, and the ability to have children. Symptoms depend on which hormones are missing.
People who have hypopituitarism usually need to take medicines for the rest of their lives to replace the missing hormones, which helps control symptoms.
The pituitary gland is responsible for making the following hormones:
- Adrenocorticotropic hormone (ACTH): This hormone stimulates cortisol production from the adrenal glands, which helps regulate blood pressure, blood sugar, inflammation, and stress response.
- Thyroid-stimulating hormone (TSH): This hormone stimulates the thyroid gland, which regulates your metabolism, energy levels, and body temperature.
- Follicle-stimulating hormone (FSH) and luteinizing hormone (LH): These hormones regulate estrogen and progesterone in women and testosterone in men. In women, FSH stimulates egg development, while LH triggers ovulation and stimulates progesterone. In men, FSH supports sperm production, while LH stimulates testosterone.
- Growth hormone (GH): This hormone targets almost all tissues in the body, especially bones and muscles, and stimulates growth in children. It regulates body composition, muscle mass, bone mineral density, and metabolism in adults.
- Prolactin: This hormone stimulates milk production after childbirth and supports women in breastfeeding.
- Antidiuretic hormone (ADH): Also known as vasopressin, this hormone regulates water balance and blood pressure, ensuring you neither lose nor retain too much water.
When the pituitary gland isn’t working well, other glands don’t get their instructions, and bodily functions like blood pressure, metabolism, and fertility are unregulated. Meanwhile, the body loses its ability to respond to stress and to change. This is why diagnosing hypopituitarism early is crucial.
When hypopituitarism affects only one hormone, it’s known as isolated pituitary deficiency. When it’s two or more hormones, it’s known as multiple pituitary hormone deficiency. When all pituitary hormones are affected, this is known as panhypopituitarism.
What causes hypopituitarism?
A pituitary tumor is the most common cause of hypopituitarism. Other causes include surgery, radiation, inflammation (also known as hypophysitis), traumatic brain injury (TBI), empty sella syndrome, and severe blood loss during or after childbirth. Sometimes, the cause of hypopituitarism is unknown—this is called idiopathic hypopituitarism.
While most cases of hypopituitarism develop later in life, the condition can be present at birth (this is called congenital hypopituitarism, and it is uncommon).

Hypopituitarism Symptoms
Hypopituitarism symptoms are multifold because the pituitary gland influences so many internal systems. Ultimately, the symptoms you experience will depend on which hormone or hormones are affected. Your age and sex, as well as what’s causing your hypopituitarism, will also influence symptoms.
If you or someone you know has hypopituitarism, you might experience a combination of the following:
- Fatigue and weakness: A common early symptom of hypopituitarism, fatigue and feelings of weakness are caused by low ACTH (low cortisol), low thyroid hormone, low sex hormones, or GH deficiency.
- Unexplained weight changes: Weight gain or loss without a change in diet or activity level can be caused by low thyroid hormone or GH deficiency.
- Cold intolerance: Feeling cold or often needing extra layers outside of seasonally cold weather can be a symptom of low thyroid hormone.
- Low blood pressure or dizziness: Feeling dizzy, especially when standing, or having consistently low blood pressure results from low ACTH and cortisol.
- Mood and cognitive changes: An unshakeable brain fog, not being able to concentrate, or experiencing prolonged bouts of feeling down or periods of depression are often linked to low thyroid, sex hormones, low ACTH, and cortisol or GH deficiency.
- Menstrual changes or fertility issues: Irregular or missed periods and difficulty getting pregnant may be due to low LH and FSH, which affect estrogen and, in turn, ovulation in women. In men, low LH and FSH can result in low sperm count, which causes male infertility.
- Loss of libido or sexual dysfunction: A reduced sex drive, vaginal dryness in women, and erectile dysfunction in men are typically associated with low LH or FSH.
- Increased urination and thirst: Excessive thirst accompanied by frequent urination can be caused by low ADH, or vasopressin, and can lead to dehydration if left unmanaged.
- Slow growth in children: The main symptom of GH deficiency, slow growth in children can also lead to delayed puberty.
These symptoms can develop very gradually, making a hypopituitarism diagnosis easy to miss without proper testing. If you notice multiple systems affected—for example, your energy levels, weight, mood, and menstrual cycle—it’s worth consulting with your healthcare professional and considering hormone testing. Early detection and treatment can prevent complications and improve outcomes.
Hypopituitarism Diagnosis
Diagnosing hypopituitarism involves careful symptom evaluation, blood tests to check hormone levels, and imaging studies to examine the pituitary gland.
Doctors may use the following exams to diagnose hypopituitarism:
- Physical and neurological exam: First, your healthcare provider will ask specific questions about your energy levels, appetite, weight changes, menstrual history, fertility, and sexual function, as well as history of head trauma, brain surgery, or cancer treatment. Next, they’ll complete a physical examination and visual field assessment.
- Magnetic Resonance Imaging (MRI): An MRI provides detailed images of the pituitary gland and its surrounding structures. In the case of hypopituitarism, an MRI is highly effective at distinguishing inflammation, structural damage, or soft tissue characteristics of tumors, as well as evaluating the size and shape of the pituitary gland and stalk.
- Blood tests: These tests are crucial to determine which hormones are low and whether the problem comes from the pituitary gland or the glands it controls, like the thyroid or adrenal glands. Hormone blood tests typically include ACTH and cortisol, TSH and free T4, LH, FSH, estradiol, testosterone, IGF-1, prolactin, and electrolyte levels.
- Stimulation tests: If your blood test results are unclear or bordering on hypopituitarism, you may require stimulation testing. These tests determine the reserve capacity of your hormone systems and how your body responds when it’s asked to produce hormones like ACTH or GH. Stimulation tests are often done in a hospital setting, as they can require close coordination with an endocrinologist.
Depending on your symptoms and results, your provider may also request visual field testing to determine if a pituitary tumor has damaged the optic nerves and caused vision problems, and ADH or vasopressin testing if there are signs of arginine vasopressin deficiency (diabetes insipidus).
Hypopituitarism Treatment
Treatment for hypopituitarism depends on which hormones are affected and the underlying cause, and can include hormone replacement therapy, surgery, radiation therapy, or another targeted approach. Each treatment aims to return the pituitary gland to its normal function.
Nonsurgical Treatments
Nonsurgical treatments are the frontline approach for hypopituitarism. Endocrinologists treat most hypopituitarism patients successfully with hormone replacement therapy tailored to their hormone deficiencies. Most people can continue to lead full and active lives by replacing their missing hormones.
Hormone replacement therapy can treat a range of deficient hormones, including:
- Steroid hormone replacement: If your pituitary gland doesn’t produce enough ACTH, your adrenal glands don’t make enough cortisol. Common medications for cortisol replacement include hydrocortisone and prednisone, both of which can be taken orally. It’s important to note that missing doses of a cortisol replacement can lead to adrenal crisis, a life-threatening condition. Cortisol replacement patients should carry a medical alert ID and an emergency injection kit.
- Thyroid hormone replacement: Low thyroid-stimulating hormone (TSH) means your thyroid is underactive, affecting your energy levels and growth. To treat this, levothyroxine (T4) is taken orally once daily. Free T4 levels must be tested to guide any dose adjustments.
- Sex hormone (estrogen/testosterone) replacement: A deficiency in LH and FSH leads to low sex hormones, which in turn affect sexual function, fertility, bone health, and mood for men and women. In women, doctors prescribe estrogen with or without progesterone in the form of pills, patches, gels, or vaginal suppositories. In men, testosterone is available in the form of injections, patches, gel, or pellets. Both hormone therapies help restore libido, energy, and sexual function, as well as preserve bone density. It’s important to note that sex hormone replacement cannot restore fertility—a different series of hormone therapy is required to stimulate ovulation or sperm production.
- Growth hormone replacement: A GH deficiency significantly affects growth in children and can cause fatigue, poor quality of life, and muscle loss in adults. To treat this, recombinant human growth hormone, or somatropin, is injected under the skin daily to promote growth and improve body composition, energy, and metabolism. Not all adults with GH deficiency require treatment; doctors prescribe it on a case-by-case basis.
- Antidiuretic hormone (ADH) replacement: In arginine vasopressin deficiency (diabetes insipidus), where the kidneys can’t conserve water, ADH or vasopressin replacement controls the body’s water balance. Doctors prescribe desmopressin as an oral tablet, nasal spray, or injection. ADH replacement is necessary only when the posterior pituitary gland is affected.
Hormone replacement therapy is not a one-size-fits-all treatment—even with these unique hormone replacement therapy treatments, some individuals may still experience fatigue, mood changes, or decreased sexual function. Treatment is often lifelong; hormones are adjusted based on symptoms and regular blood tests.
Your overall quality of life will improve once you and your healthcare team find the most effective treatment strategy for your condition.
Other nonsurgical treatments for hypopituitarism can include:
- Regular monitoring for radiation therapy-induced damage;
- Discontinuing immunotherapy or switching treatments if immune checkpoint inhibitors are causing severe symptoms.
Surgical Treatments
A neurosurgeon is consulted for hypopituitarism only when there’s a structural issue interfering with pituitary gland function—for example, a pituitary tumor that’s pressing on nearby tissue, compressing the optic nerves and causing vision problems.
The exact surgery will depend on the tumor’s size, type, location, and impact on surrounding tissues, and can include:
- Transsphenoidal surgery: The most common surgical approach for a pituitary tumor is transsphenoidal surgery. This is when a neurosurgeon reaches and removes the tumor through the nasal passages and the sphenoid sinus using a small surgical instrument and an endoscope. Transsphenoidal surgery works best on small to medium-sized pituitary tumors confined to the sella turcica—the bony compartment of the pituitary gland—and leaves no scar. It also minimizes the risk of complications and offers a faster recovery.
Your hormone function might recover after surgery, but you may require lifelong hormone replacement and management.
Whether the proper treatment is hormone replacement therapy or surgery, most people with hypopituitarism can live normal lives.
One Central Location with Multiple Treatment Options
At Barrow Neurological Institute’s renowned Pituitary Center, we treat people with pituitary tumors and disorders in one robust location. And because our doctors and nurses treat more people with pituitary disorders than any other team in the Southwest U.S., you can rest assured that you’ll be in very experienced hands.
Common Questions
How common is hypopituitarism?
Hypopituitarism is considered a rare condition in the U.S., but it’s likely underdiagnosed. The prevalence of hypopituitarism in the general U.S. population is between 45 and 50 cases per 100,000 people, or about 150,000 to 170,000 Americans.
Who gets hypopituitarism?
The most common causes of hypopituitarism are pituitary tumors, traumatic brain injury (TBI), and surgery on or radiation therapy to the pituitary gland. Pituitary tumors predominate, accounting for up to 70 percent of cases.
Doctors diagnose a large percentage of hypopituitarism cases in middle-aged adults, but hypopituitarism can occur at any age. There’s a slight predominance in females, particularly when linked to autoimmune causes or pregnancy. Recent years have seen more cases of hypopituitarism linked to cancer immunotherapies and TBIs.
What is the prognosis for someone with hypopituitarism?
With proper treatment, the prognosis for someone with hypopituitarism is favorable. Most people can live a normal or near-normal lifespan with prompt identification of hormone deficiencies and adequate monitoring of hormone replacement therapy.
In contrast, pituitary tumors that trigger hypopituitarism may require surgery or radiation, and long-term outcomes will depend on tumor control and pituitary gland recovery. Hypopituitarism related to traumatic brain injury may improve over time in some cases, but can also worsen if missed.
If you have hypopituitarism that affects your ACTH levels, being educated on adrenal crisis will be vital in preventing an emergency, especially during illness, injury, surgery, or in the absence of stress-dose steroids. Proper emergency planning, such as carrying injectable hydrocortisone, significantly reduces this risk.
Can hypopituitarism be prevented?
Hypopituitarism cannot be entirely prevented, especially when it’s the result of an autoimmune reaction, pituitary tumor, or a genetic condition.
However, some causes are preventable or at least manageable, and early intervention can reduce the risk of severe hormone loss. Ways to reduce the risk of hypopituitarism in these settings can include:
- Preventing and monitoring care after a traumatic brain injury (TBI): Recognized as a significant cause of hypopituitarism, you can dramatically reduce your risk of TBI by always wearing a seat belt in the car or a helmet during impact activities and enlisting fall-prevention measures when heights are involved. Enforcing safe sports practices and post-concussion protocols in sports is also critical. For moderate-to-severe TBI survivors, hormone monitoring is crucial to prevent hypopituitarism.
- Minimizing exposure during pituitary surgery or radiation therapy: When surgery or radiation therapy is required, prevention will focus on reducing your exposure to unnecessary radiation through regular follow-up imaging and hormone testing.
- Promptly treating immunotherapy-induced hypophysitis: To reduce your risk of symptoms and complications from hypopituitarism caused by checkpoint inhibitors in cancer treatment, regular monitoring of hormone levels can catch early hormone variations and prompt hormone replacement therapy.



