
Medulloblastoma
Overview
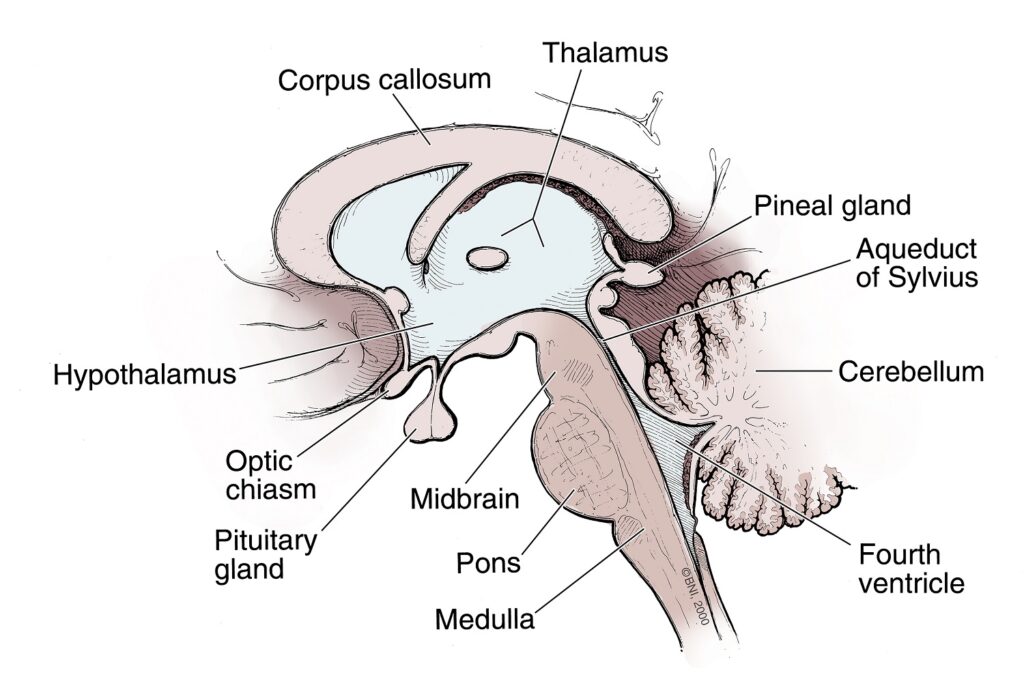
A medulloblastoma is a cancerous brain tumor that starts in the cerebellum, at the base of the skull. The cerebellum controls balance, coordination, and several complex motor functions.
Medulloblastomas are often fast-growing and can spread to other areas of the brain or spinal cord through cerebrospinal fluid (CSF), a watery liquid that protects both organs.
Medulloblastomas belong to a group of cancers called embryonal tumors, or growths that start from brain cells left over from fetal development. They’re classified by two criteria:
- Their microscopic or histologic appearance
- Their molecular subtype, or the tumor’s genetic characteristics
These tumors are more common in children, but doctors diagnose up to 200 new cases a year in adults in the United States. Knowing a medulloblastoma’s histologic and molecular subtype is critical because it helps guide diagnosis, treatment, and overall prognosis.
The histologic subtypes of medulloblastoma include:
- Classic medulloblastoma: This is the most common histologic subtype. Under a microscope, these tumor cells appear small, round, and blue and are densely packed, with minimal space between them.
- Desmoplastic or nodular medulloblastoma: This subtype is characterized by areas of dense cells alternating with less dense, more organized regions, creating a “nodular” appearance.
- Large-cell medulloblastoma: These tumor cells are larger and more uniform in appearance than in other subtypes. They tend to be arranged in solid sheets with large, round nuclei.
- Anaplastic medulloblastoma: This tumor subtype shows highly abnormal, aggressive-looking cells with large, irregular nuclei. This histologic subtype is often paired with more aggressive molecular subtypes, like Group 3 below.
The molecular subtypes of medulloblastomas include:
- WNT: This subtype is generally found in the midline of the cerebellum, often near the brainstem, and is defined by mutations in the WNT signaling pathway, hence its name. WNT medulloblastomas represent about 10 percent of all medulloblastomas.
- SHH: This subtype is frequently found in the outer portions of the cerebellum and is associated with mutations in the SHH signaling pathway. SHH medulloblastomas make up around 30 percent of all medulloblastomas.
- Group 3: This subtype is often spotted in the midline of the cerebellum and is the most aggressive subtype, accounting for approximately 25 percent of medulloblastomas.
- Group 4: This is the most common subtype—representing up to 40 percent of medulloblastomas—yet it’s the least understood at a molecular level. Like Group 3, these tumors are often found in the midline of the cerebellum but are not as aggressive.
While complex, these two systems combine to create a panoramic understanding of medulloblastoma and help guide more effective, personalized treatments.
What causes medulloblastomas?
The exact cause of medulloblastomas isn’t fully understood. What researchers do know is that genetic mutations or abnormalities in the DNA of developing brain cells can lead to tumor formation.
Additionally, some genetic conditions can increase the risk of developing medulloblastoma. These include:
- Gorlin syndrome: Also known as nevoid basal cell carcinoma syndrome, this genetic condition increases the risk of developing both cancerous and noncancerous tumors. People with Gorlin syndrome have around a five percent chance of developing a medulloblastoma.
- Turcot syndrome: This rare genetic disorder causes small growths or polyps in the intestines that lead to colorectal cancer and increases the risk of brain or spinal cord tumors, such as a medulloblastoma or pituitary adenoma.
- Li-Fraumeni syndrome: This genetic condition increases the risk of multiple cancers, including medulloblastomas.
Ultimately, most cases of medulloblastoma happen in people without any known genetic cause.

Medulloblastoma Symptoms
Symptoms of a medulloblastoma depend on the tumor’s size, location, and whether it has spread to other parts of the brain or spinal cord.
The symptoms you or a loved one might experience if you have medulloblastoma include:
- Headaches, especially in the morning or after lying down: One of the most common symptoms is headaches, which are often worse in the morning or after lying down due to increased pressure in the brain.
- Nausea and vomiting: This symptom will often happen alongside headaches because of the increased pressure from the tumor.
- Balance and coordination problems: Because the cerebellum is responsible for balance and coordination, people with medulloblastomas can experience stumbling, trouble walking, or difficulty with fine motor tasks like writing.
- Vision problems: Blurring or double vision can happen when the tumor creates pressure on the nerves that control eye movement.
- Fatigue and drowsiness: Increased pressure from tumor growth can lead to general fatigue, drowsiness, or lethargy.
- Behavioral changes: Personality or behavioral changes can manifest as new or unusual emotional states, like changes in judgment, aggressiveness, irritability, or loss of initiative. This is especially noteworthy in children.
- Hydrocephalus: When a tumor blocks the flow of cerebrospinal fluid (CSF) and leads to a buildup of fluid in the brain, hydrocephalus can occur. This condition causes severe headaches, nausea and vomiting, changes in behavior or consciousness, and an increase in head size in infants.
- Back pain or difficulty walking: When a medulloblastoma spreads to the spinal cord, it can result in back pain, leg weakness, or even loss of bladder and bowel control.
- Seizures: Though less common, a new onset of seizures can occur, especially if the tumor causes significant pressure in the brain.
If you or your loved one is exhibiting persistent or worsening symptoms, it’s vital you see a healthcare provider. Early diagnosis of medulloblastomas can lead to better outcomes after treatment.
Medulloblastoma Diagnosis
Diagnosing a medulloblastoma often involves multiple steps, beginning with an evaluation and followed by a series of imaging and diagnostic tests.
Doctors commonly use these exams, tests, and imaging studies to find a diagnosis:
- Physical and neurological exam: First, your healthcare provider will ask about your symptoms, overall health, and any risk factors you might have for a medulloblastoma, including genetic conditions or family history. Next, they’ll complete a neurological examination to assess neurological function, balance, coordination, vision, hearing, reflexes, and strength.
- Magnetic Resonance Imaging (MRI): An MRI is the leading imaging test to detect a medulloblastoma. An MRI provides detailed images of your brain and helps identify tumor location, size, and characteristics. A contrast agent may also be injected during your MRI to highlight the tumor and help differentiate it from other tissues.
- Spinal MRI: A spinal MRI may also be ordered to check for possible tumor spread in your spinal cord, as medulloblastomas can spread through cerebrospinal fluid.
- Computed Tomography (CT): A CT scan can help evaluate a tumor’s size and location using X-rays to create detailed cross-sectional images. That said, an MRI is generally the first choice in neuroimaging for medulloblastomas.
- Biopsy: If your imaging results suggest a tumor, a conclusive diagnosis will require a biopsy. A biopsy establishes an exact diagnosis by removing a small tissue sample from the tumor, either surgically or through stereotactic biopsy, and sending it to a pathology laboratory for analysis. There, the tissue is examined under a microscope to determine the type of cells present and whether they’re cancerous or noncancerous. In the case of medulloblastomas, a biopsy is crucial as the tumors have different subtypes, and your treatment plan and prognosis will vary based on this subtype.
- Molecular testing: Tissue from your biopsy is frequently tested for specific genetic or molecular features because doctors classify medulloblastomas into four molecular subgroups. Molecular testing also helps determine the best treatment approach.
- Lumbar puncture: Also known as a spinal tap, this test collects a sample of cerebrospinal fluid from around the spinal cord to test for cancer cells. A lumbar puncture is most often done after surgery, as increased pressure in the brain before surgery can make this procedure dangerous.
Your care team may run additional tests, such as blood panels or hearing exams, to provide more context before starting treatments and to establish a baseline hearing reference. This is because treatments for medulloblastomas can affect hearing.

Medulloblastoma Treatment
A treatment plan for a medulloblastoma will depend on several factors, such as the tumor’s histological and molecular subtype, its location, whether it has spread, and a person’s age.
Most often, treatment involves a combination of therapies designed to remove the tumor, destroy any remaining cancer cells, and prevent the cancer from spreading or recurring. While medulloblastomas are serious brain tumors, they’re also treatable—especially when diagnosed early.
Surgical Treatments
Surgery is usually the first step in medulloblastoma treatment. The goal of surgery is to remove the entire tumor, but depending on its size and location, this may not be feasible without risking damage to critical brain structures. That said, even partial removal can reduce your symptoms and improve the effectiveness of other treatments.
- Gross Total Resection (GTR): In this procedure, a surgeon aims to remove the whole tumor, achieving what’s known as gross total resection. This is considered the ideal outcome and offers the best chance of long-term survival. In many cases, gross total research is achievable, mainly when the tumor is localized and hasn’t spread to other parts of the brain or spine.
- Subtotal Resection: If the tumor is near essential structures like the brainstem or nerves that control vital functions, removing the whole tumor may not be possible without risking significant damage. In such cases, a subtotal resection is done, meaning that part of the tumor is left behind. However, radiation and chemotherapy can target the remaining tumor cells.
During surgery, neurosurgeons often use intraoperative MRI and neuro-navigation systems to guide the tumor resection procedure more precisely. Intraoperative neurophysiological monitoring may also be used to ensure critical functions are preserved. In addition to the surgical removal of the tumor, your surgeon may recommend a shunt to help drain any cerebrospinal fluid buildup.

Nonsurgical Treatments
After surgery, patients usually undergo radiation therapy and chemotherapy to destroy any remaining cancer cells and prevent them from coming back.
Nonsurgical treatments for medulloblastoma include:
- Radiation therapy: Radiation therapy uses precisely aimed beams of radiation to destroy tumors in the body. While it doesn’t remove the tumor, radiation therapy damages the DNA of the tumor cells, which then lose their ability to reproduce and eventually die. Radiation therapy is often used after surgery—particularly for high-grade medulloblastomas—to reduce the risk of recurrence. However, radiation therapy is carefully considered in children because it can affect brain development. Radiation is most commonly delivered to the brain and spine, which is called cranio-spinal radiation. This is because the cancer cells tend to float microscopically throughout the central nervous system.
- Chemotherapy: Chemotherapy is typically used after surgery with radiation, after radiation, or on its own, especially in younger children, to delay radiation. Oncologists can give chemotherapy as a pill, an intravenous (IV) infusion, or sometimes directly into the cerebrospinal fluid to target cancer cells in the brain and spine. Common chemotherapy drugs for medulloblastomas include Carboplatin, Lomustine, Cisplatin, Vincristine, Cyclophosphamide, and Etoposide. For high-risk patients, chemotherapy is often more aggressive, particularly in those whose tumors have spread or could not be entirely removed during surgery.
- Molecular targeted therapy: A newer area of treatment, targeted therapies are designed to attack specific molecules or pathways involved in cancer growth and are often based on medulloblastoma subtypes.
After treatment is completed, long-term follow-up care is mandatory to monitor for tumor recurrence and manage any long-term side effects. Regular MRIs check for signs of returning tumors, and for children, cognitive, neurological, and endocrine assessments are also often done to assess developmental delays or challenges as a result of treatments.
One Central Location with Multiple Treatment Options
At Barrow Neurological Institute’s world-class Brain and Spine Tumor Program, we treat people with complex tumors like medulloblastomas in one robust, full-service location. Our sophisticated multidisciplinary team—neurosurgeons, head and neck surgeons, neuro-oncologists, medical oncologists, and radiation oncologists, to name a few—can offer you the latest treatments for head and neck cancers, including metastatic cancers.
We also give our patients access to various neuro-rehabilitation specialists to enhance their physical abilities, maximize independence, and support their mental health. Since gliomas—particularly high-grade ones—can significantly impact quality of life, supportive care is crucial.
Neuro-rehabilitation can include physical therapy to help you regain strength and balance, speech therapy to support speaking and expressing thoughts, and occupational therapy to aid in managing daily activities like bathing, dressing, and using the bathroom. Treating a brain or spinal cord tumor is about more than extending your life—it’s also focused on enhancing your quality of life.
Clinical Trials
In partnership with the Ivy Brain Tumor Center, Barrow Neurological Institute is proud to be one of the country’s largest sites for brain tumor clinical trials.
Clinical trials are part of the cancer research process to determine if new treatments are safe, effective, or even better than the current standard treatment. Although not yet FDA-approved, clinical trials can be the best option for those with difficult-to-treat tumors to improve the odds of finding an effective treatment for them and for future patients. If you’re diagnosed with a glioma—especially one with an aggressive grade like a Grade 3 medulloblastoma—you may be a candidate.
To search for clinical trials that are now enrolling, visit here.
Common Questions
How common are medulloblastomas?
Each year, doctors diagnose approximately 500 new cases of medulloblastoma in the United States.
Although medulloblastomas are rare, they are the most frequently diagnosed pediatric malignant brain tumors, accounting for close to 20 percent of all pediatric brain tumors. Moreover, their impact is significant because of their aggressive nature and the degree of treatment involved. Up to 200 new cases each year in the U.S. are in adults.
Who gets medulloblastomas?
As the most common malignant brain tumor in children, most cases of medulloblastomas are diagnosed between the ages of 3 and 9 years old, and boys are slightly more affected than girls.
Medulloblastomas account for only about one to two percent of all adult brain tumors. Most adult medulloblastomas are diagnosed between the ages of 20 and 44. However, they can occur at any age.
What is the prognosis for those with medulloblastomas?
The survival rates for medulloblastoma depend on several factors, including tumor size, the extent to which the tumor can be removed, whether it has spread to other parts of the body, and a person’s age.
Children generally have a better prognosis than adults. However, those under three years old may have a slightly worse prognosis due to challenges in treatment, particularly with the use of radiation. With modern treatments, many children diagnosed with medulloblastomas can live long lives—in fact, up to 75 percent of children treated with surgery, radiation, and chemotherapy survive into adulthood.
The prognosis for adults with medulloblastoma is generally worse. The five-year survival rate is between 50 to 60 percent, but this can vary depending on the tumor subtype and extent.
Based on the four molecular subtypes, the following prognoses have been observed:
- WNT: This is the most favorable medulloblastoma subtype with long-term survival rates of 90 percent or higher, especially in children.
- SHH: This subtype’s prognosis is generally better in children but worse in adults. Treating infants and children under three years old with the SHH subtype can be challenging, but the survival rates are still promising.
- Group 3: This subtype has a poor prognosis due to its aggressive nature and greater likelihood of spreading, or metastasizing, to other parts of the brain or spine. Survival rates are as low as 50 percent.
- Group 4: This subtype has a middle-of-the-ground prognosis, with survival rates generally between Group 3 and SHH or WNT. Depending on how much the tumor has spread, survival rates range between 60 and 75 percent.
Can medulloblastomas be prevented?
Medulloblastomas cannot be entirely prevented, as their exact cause is poorly understood. Most happen sporadically, meaning they develop without known risk factors or environmental triggers. And unlike other cancers, exposure to toxins, chemicals, or radiation has not been linked to an increased risk of medulloblastomas.
However, some genetic conditions may slightly increase your risk of developing a medulloblastoma, including:
- Gorlin syndrome: Also known as nevoid basal cell carcinoma syndrome, this genetic condition increases the risk of developing both cancerous and noncancerous tumors. People with Gorlin syndrome have around a five percent chance of developing a medulloblastoma.
- Turcot syndrome: This rare genetic disorder causes small growths or polyps in the intestines that lead to colorectal cancer and increases the risk of brain or spinal cord tumors, such as a medulloblastoma or pituitary adenoma.
- Li-Fraumeni syndrome: This genetic condition increases the risk of multiple cancers, including medulloblastomas.
If you or your loved one has a family history of these genetic conditions, genetic counseling and regular monitoring by specialists can help. Additionally, recognizing symptoms early and seeking prompt medical evaluation can lead to an earlier diagnosis, improving the chances of successful treatment.













