
Resection of Vertebral Osteoid Osteoma with Frameless Stereotactic Assistance: Case Report
Jeffrey S. Henn, MD
Vivek Deshmukh, MD
Volker K. H. Sonntag, MD
Division of Neurological Surgery, Barrow Neurological Institute, St. Joseph’s Hospital and Medical Center, Phoenix, Arizona
Abstract
A vertebral osteoid osteoma was localized and resected with the assistance of spinal frameless stereotaxy. The stereotactic system helped to localize the lesion precisely, to verify the local anatomy, and to insure a complete resection. Traditionally, frameless stereotaxy has been used in the treatment of intracranial lesions, but spinal applications have become more common.
Key Words: osteoid osteoma, spinal frameless stereotaxy
Frameless stereotaxy can be a useful adjunct in spinal surgery. This case describes the application of frameless stereotaxy to the resection of a vertebral osteoid osteoma.

Illustrative Case
A 17-year-old male had suffered progressively worsening lower back pain for 2 years. The patient’s pain was typically worse at night and improved after he took aspirin. At evaluation, he was taking as many as 10 aspirin tablets/day. His medical history was otherwise normal. His physical examination revealed significant tenderness to palpation over the left lower lumbar region. He also had a visible scoliotic deformity. His motor examination showed 5/5 strength throughout all muscle groups, and his sensory and reflex examinations were normal.
Plain radiographs of his lumbar spine demonstrated a mild scoliotic deformity and enlargement of the left L4 pedicle. A bone scan demonstrated abnormal uptake in the region of the L4 pedicle and facet (Fig. 1).
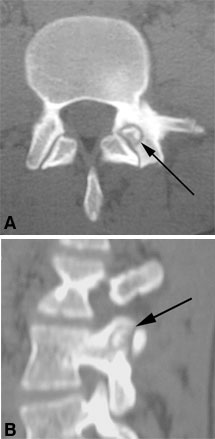
Computed tomography (CT) of the lumbar spine showed a lesion in the left L4 superior facet and significant sclerotic changes of the L4 pedicle (Fig. 2). The patient’s clinical history, presentation, and imaging studies were considered consistent with the diagnosis of osteoid osteoma. Based on his worsening back pain, the decision was made to proceed with surgical resection.
Spinal frameless stereotaxy was used to assist with localization and resection because the lesion was small, completely encased in bone, and not visible directly. Before surgery, the patient underwent fine-cut, noncontrast CT, and the data were transferred to the StealthStation frameless stereotactic system (Medtronic Surgical Navigation Technologies, Louisville, CO).
After general endotracheal anesthesia was induced, the patient was placed in the prone position. A midline incision was centered over the L3-L4 interspace. A unilateral exposure was performed on the left to expose the spinous processes and laminae of L3 and L4 and the L3-L4 facet joint. The operating microscope was used.
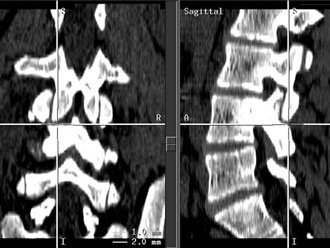
A series of readily identifiable landmarks were used to perform paired-point registration. In each case, an anatomical point was identified on the exposed spine, and the corresponding point was identified on the radiographic imaging data (Fig. 3).
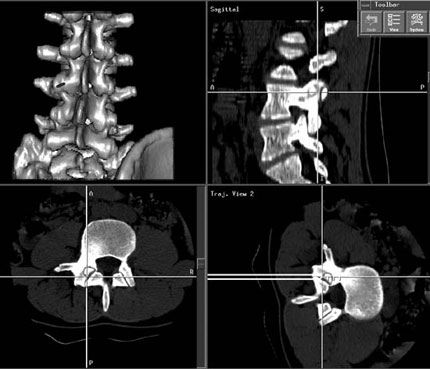
After registration was satisfactory, frameless stereotactic navigation and anatomic landmarks were used to localize the lesion. To access the lesion, the inferior L3 facet was removed using a high-speed air drill. After the facet synovium was removed, the lesion was encountered (Fig. 4).
The lesion was resected with a combination of curettes and rongeurs. The remaining portion of the left superior L4 facet and the sclerotic region of the L4 pedicle were also removed. Great care was taken to protect the nerve roots of L3 and L4. After hemostasis was obtained, the wound was closed in routine fashion. The final pathologic diagnosis of the lesion and bone was consistent with osteoid osteoma. Postoperative CT confirmed complete lesion resection. The patient’s postoperative course was uneventful. By postoperative Day 1, the patient was experiencing much less pain than he had before surgery.
Discussion
This patients’ clinical and radiographic studies were classic for vertebral osteoid osteoma. Based on the size of the lesion and its location within the bone, the decision was made to use frameless stereotaxy as a surgical adjunct. Although our patient’s osteoid osteoma likely could have been resected without the aid of frameless stereotaxy, it was a useful adjunct in this case. No difficulties were encountered, and the technique helped to localize the lesion precisely and to define the local regions of normal and abnormal anatomy. Frameless stereotaxy was also useful to verify that the lesion had been resected completely.
Frameless stereotaxy is often used in the treatment of intracranial lesions. Because of the relative difficulty of registration, mobility between the vertebral segments, and need for definable anatomic landmarks, it is less commonly employed in spinal procedures. Frameless stereotaxy, however, can be a useful adjunct for placing spinal instrumentation and for resecting certain spinal tumors.[1]
References:
- Karahalios DG, Apostolides PJ, Geldmacher TR, et al: Image-guided spinal surgery. Operative Techniques in Neurosurgery 1(3):104-112, 1998
