
Endovascular Treatment of Orbital Lesions
Authors
Neil M. Borden, MD
Mazen H. Khayata, MD†
Bruce L. Dean, MD
Richard A. Flom, MD
Adel M. Medhkour, MD‡
Burton P. Drayer, MD
Robert F. Spetzler, MD‡
Division of Neuroradiology, ‡Division of Neurological Surgery, Barrow Neurological Institute, Mercy Healthcare Arizona, Phoenix, Arizona
†Current address: Arizona Heart Institute, Phoenix, AZ
Abstract
During a 2-year period, 17 patients with vascular abnormalities that involved the orbital contents were evaluated. Nine patients had carotid-cavernous sinus fistulae (CCSF) (6 direct, 3 indirect). Three patients had orbital cavernous venous malformations, two patients had traumatic arteriovenous fistulae, two patients had orbital-facial arteriovenous malformations, and one patient had a large olfactory groove meningioma supplied by the ophthalmic artery. All patients, except for two with asymptomatic venous malformations, underwent endovascular therapy. The nine patients with CCSFs and the two untreated patients with venous malformations are excluded from discussion. The remaining six patients underwent endovascular treatment, which included direct puncture and ophthalmic artery embolization. A multidisciplinary approach (surgery, radiation, or both) was used in four of the six patients. Favorable outcomes were achieved in all six patients, and no neurologic complications resulted from the endovascular procedures. A wide variety of vascular lesions may involve the orbit directly or indirectly. Endovascular techniques can be helpful in treating these lesions, which often require a multidisciplinary approach to achieve the most satisfactory results. Under proper conditions, direct puncture techniques and superselective ophthalmic artery embolization may be employedin treatment protocols.
Key Words : arteriovenous malformation, carotid-cavernous sinus fistula, endovascular, meningioma, ophthalmic artery, orbit
Endovascular treatment has emerged as an innovative and effective method for treating vascular lesions of the central nervous system (CNS). This technique, however, has not yet been used in many CNS locations that have delicatestructures. One such frontier, the orbit, has been avoided in lieu of more conservative approaches to treatment.Advances in guidewire and microcatheter technology, in addition to improved digital-subtraction angiography (DSA) and road-mapping techniques, now allow the surgical neuroangiographer to navigate previously unreachable territories with limited risk. It is possible to place microcatheters into the ophthalmic artery distal to the central retinalartery—a placement that is a prerequisite to safe embolization.3,9,10
Embolization can be useful in definitive (primary) treatment, as well as being an adjunct to surgery and radiation in treating vascular abnormalities of the orbital contents. A variety of vascular malformations can occur in the orbit, including high-flow arteriovenous malformations (AVMs), slow-flow dural-vascular malformations, and cavernous-venous malformations. Carotid-cavernous sinus fistulae (CCSF) can involve the orbit indirectly via orbital venous drainage.2,11 Orbital and peri-orbital neoplasms parasitizing blood flow from orbital arteries can also occur. Although endovascular treatment of such lesions is possible under safe conditions using proper techniques, embolization through the ophthalmic artery can be a contraindication to treatment because of the danger of inducing blindness by occluding the retinal artery. However, if the microcatheter can be placed distal to the central retinal artery, embolization through this route can be performed cautiously. Unfortunately, the extreme tortuosity of the ophthalmic artery may preclude distal catheterization and embolization via this route. Symptomatic orbital cavernous-venous malformations can be treated with low morbidity by direct puncture and injection of a sclerosing agent. This article summarizes our experience in treating a variety of vascular lesions involving the orbital contents.
Methods and Materials
Between April 1992 and August 1994, 17 patients with vascular lesions involving the orbital contents were evaluated by the Endovascular Service. Their medical records and imaging studies were reviewed retrospectively. Of the 17 patients, 9 had CCSFs: 6 patients had direct CCSFs and 3 patients had indirect CCSFs (dural AVMs). All 17 patients, except two with asymptomatic orbital venous malformations, were treated by endovascular methods. The nine patients with direct and indirect CCSFs and the two untreated asymptomatic patients with orbital cavernous-venous malformations are excluded from further discussion. The remaining six patients underwent diagnostic angiography and endovascular treatment (Table 1). A multidisciplinary approach utilizing surgery, radiation, or both was used to treat four of these six patients (Table 2).
Table 1
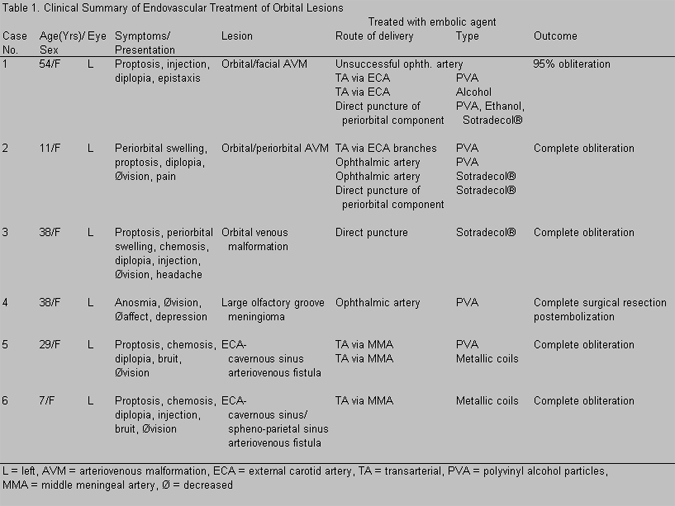
Table 2
All angiograms and endovascular treatments were performed using DSA and road-mapping techniques. Of the six patients, five (Cases 1, 2, 4, 5, and 6) underwent angiography and embolization via a transfemoral, transarterial approach. Three patients (Cases 1, 2, and 3) underwent direct puncture of their lesions using 21- (Cases 1 and 2), 22-, and 23-gauge (Case 3) butterfly needles. In Cases 2, 3, and 4, the lesions were embolized by different combinations of Tracker 10 and Tracker 18 (Target Therapeutics, Freemont, CA) microcatheters in conjunction with Seeker, Dasher, and Taper microguidewires (Target Therapeutics, Freemont, CA). A variety of embolic agents were used in each case (Table 1). Orbital signs and symptoms of five of the six patients showed a marked overlap (Table 1). In contrast, the patient (Case 4) who had a large olfactory groove meningioma exhibited no orbital symptoms related to her lesion.
Direct Puncture Technique
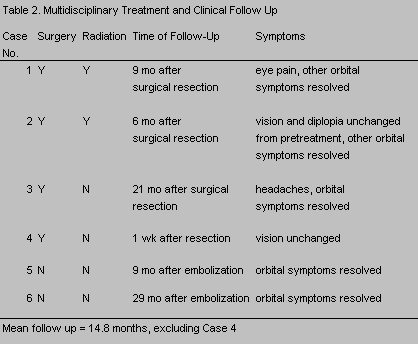
In Case 3, the venous malformation was punctured directly with 21- and 23-gauge angiocatheters. The angiocatheter was placed in a dependent position allowing backbleeding to be identified once the lesion was entered. Puncture and contrast injection were performed under fluoroscopic guidance. Nonionic contrast was instilled into the venous malformation and allowed to unfold and expand the pouch (Fig. 1A and B). An attempt was made to empty the contrast from the venous malformation before sclerosing therapy. Sotradecol® was the sclerosing agent used to treat the venous malformation of Case 3.
The peri-orbital components of the AVMs in Cases 1 and 2 were treated by direct puncture with instillation of various embolic agents (Table 1). The site for direct puncture was localized with the aid of DSA and digital roadmapping.
Avitene and gelfoam powder were used to close the needle tracts where direct puncture was used to treat the orbital venous malformation (Case 3) and the peri-orbital components of the AVMs in Cases 1 and 2.
AVMs and Peri-Orbital Neoplasm
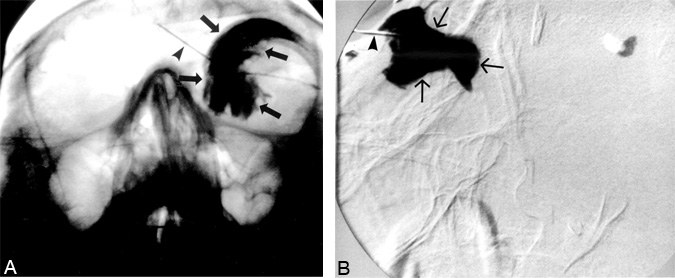
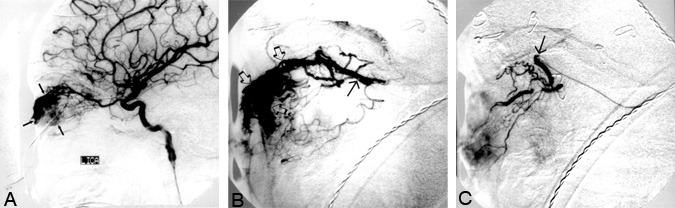
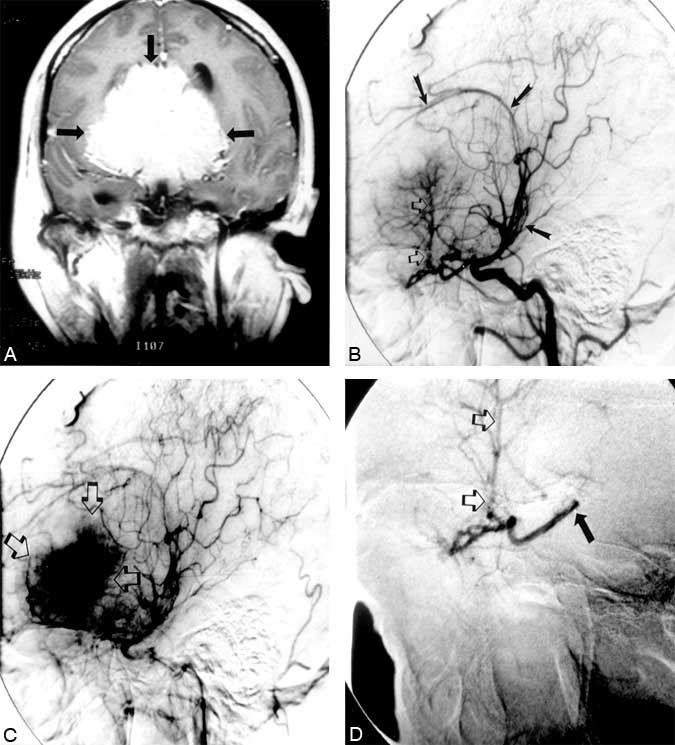
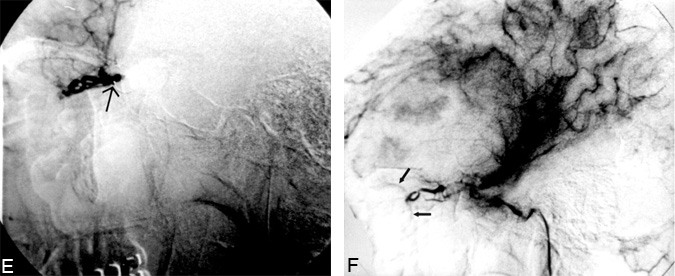
Our technique of embolization for orbital-periorbital AVMs and neoplasms required the use of microguidewire, torque-directed, and steerable microcatheters. The microcatheters were placed coaxially through a guiding catheter placed in either the external or internal carotid arteries. The dead space of the guiding catheter was flushed continuously with heparinized, pressurized saline. Digital road-mapping was necessary for safe catheterization in this region. The patient (Case 2) with an orbital/periorbital AVM underwent transarterial embolization of the external carotid artery and ophthalmic artery feeders (Fig. 2A and B). Sotradecol® (1.2 ml) was infused into the ophthalmic artery after the Tracker 10 microcatheter (Target Therapeutics, Freemont, CA) was placed beyond the central retinal artery (Fig. 2C). The Tracker 10 microcatheter and Seeker 10 microguidewire were used to embolize the ophthalmic artery supply to the large olfactory groove meningioma in Case 4 (Fig. 3A-F).
Middle Meningeal Artery Fistulae
The technique of embolization in Cases 5 and 6 required steerable, tracker (Target Therapeutic, Freemont, CA), microcatheter, microguidewire systems to gain access to the fistula. These microcatheters were placed coaxially through a guiding catheter placed in the external carotid artery. DSA and digital road-mapping were necessary for safe navigation. In both cases, metallic coils were deposited at the site of the fistulae. Case 5 required additional embolization with polyvinyl alcohol (PVA) particulates.
Results
Favorable outcomes were achieved in all six patients who underwent endovascular treatment of their orbital or peri-orbital lesion (Table 1). A multidisciplinary approach (Table 2) was required in all but two patients (Cases 5 and 6). No neurologic complications resulted from the endovascular procedures.
Orbital and Peri-Orbital Vascular Malformation
Both orbital and peri-orbital vascular malformations were treated by surgery, embolization, and radiation therapy. Embolization was performed by the transarterial route and by direct puncture in Cases 1 and 2. Endovascular treatment occurred in multiple stages in both patients. Ophthalmic artery embolization was achieved in one patient (Case 2) and attempted in the other (Case 1) with a 1.5-French flow-guided catheter and steerable Tracker 10 system. However, in Case 1 the catheter could not be placed in a safe position distal to the central retinal artery. No neurologic deficits or visual decline resulted from the superselective ophthalmic artery embolization in Case 2. This patient was cured completely with combined embolization, radiation, and surgery. In Case 1, the malformation was almost obliterated using combined endovascular, surgical, and radiation treatments.
Venous Malformation
The patient with an orbital cavernous-venous malformation (Case 3) underwent two stages of endovascular treatment. Both stages involved direct puncture of the lesion with infusion of Sotradecol® as a sclerosing therapy and were followed by surgical resection. This combined approach eliminated the malformation.
Peri-Orbital Arteriovenous Fistula with Orbital Venous Drainage
The fistulae in Cases 5 and 6 were obliterated through transarterial embolization with metallic coils. Case 5 required additional embolization with PVA, but surgery was not needed to obtain a cure.
Large Olfactory Groove Meningioma
Case 4 underwent gross total resection of her neoplasm after transarterial embolization. Embolization by superselective catheterization of the ophthalmic artery successfully devascularized the ethmoidal branches that supplied the mass. The patient’s neurologic examination and vision were unchanged after embolization. Despite successful embolization of the ophthalmic artery feeder, the estimated blood loss at surgery was 1500 ml because of the large size of the tumor and the pial supply.
Discussion
A wide variety of pathology with similar clinical symptoms can involve the vascular structures of the orbit. Vascular neoplasms and vascular malformations can involve the orbit directly or indirectly. Arteriovenous fistulae outside the confines of the orbit often have prominent orbital venous drainage. Proper diagnosis requires angiographic evaluation in conjunction with the patient’s clinical history and findings on magnetic resonance (MR) imaging or computed tomography (CT). Endovascular treatment will vary depending upon the anatomical and the pathological changes unique to the lesions and the goals of treatment. Superselective embolization through the ophthalmic artery requires careful consideration of the risks versus benefits of the procedure as well as consideration of alternative methods of treatment that might be safer.
Orbital Venous Malformation
Pure venous malformations require direct puncture techniques for endovascular management because these lesions cannot be reached through traditional transarterial or transvenous approaches.1,5,8,9 Sclerosing therapy, after direct puncture, is safe and effective for treating facial-venous malformations.1,5,8,9 Applying this technique to orbital-venous malformations therefore seems logical. However, this technique requires that the lesion have a favorable anatomic location. If this technique is to be used to treat the orbit, critical orbital structures, including the globe and optic nerve, must be avoided. Effective treatment can require multiple punctures if the venous malformation is compartmentalized. Compartmentalization may result from previous episodes of thrombosis, surgery, hemorrhage, or infection.5
Orbital/Peri-Orbital Neoplasms
Orbital and peri-orbital neoplasms may have a significant vascular supply from branches of the ophthalmic artery. Preoperative embolization of hypervascular neoplasms is an established technique in other anatomic locations.6,7 The technique is safe and effective in devascularizing tumors and lowers surgical rates of morbidity and mortality.6,7 Vascular neoplasms that derive their vascular supply from branches of the ophthalmic artery can be embolized safely only with appropriate care and meticulous techniques. Superselective catheterization of the ophthalmic artery can be achieved with steerable microguidewire-directed microcatheters. The tip of the microcatheter must be positioned distal to the central retinal artery when embolizing with small particles or liquid agents, and great care must be exerted to avoid reflux. If these guidelines are not followed and small particles or liquid embolic agents are used, blindness can result. Provocative testing with direct infusion of lidocaine into the ophthalmic artery is recommended before embolization.4 If a visual disturbance occurs, embolization from that catheter position should not be performed, or an embolic particle larger than the retinal artery should be chosen.4 In addition, a risk of mechanical damage to the ophthalmic artery with spasm, dissection, occlusion, or perforation exists. Despite these relative risks, we believe that this technique should be considered for preoperative embolization when the anatomic disposition is favorable and the risks, benefits, and alternative methods of treatment have been analyzed carefully.
Vascular Malformations
The guidelines discussed for orbital and peri-orbital neoplasms also apply to the treatment of orbital and peri-orbital vascular malformations. In these cases, however, the increased blood flow through the orbit with the associated increase in the caliber of the ophthalmic artery may provide an easier and safer access for embolization. Orbital vascular malformations are rare and often part of a more extensive orbital-facial malformation.3,10 Curative embolization of vascular malformations in this location may be impossible.9 However, preoperative embolization can markedly reduce operative blood loss as well as decrease the volume of the lesion. The presence of intraluminal clot and embolic particles can assist the surgeon in identifying the lesion at the time of operation.3 For vascular malformations and neoplasms, surgery should follow soon after embolization to diminish the development of collaterals.3
Peri-Orbital Arterial Venous Fistulae with Orbital Venous Drainage
The two patients with arteriovenous fistulae that involved the middle meningeal arteries had histories of both recent (Case 6) and remote (Case 5) trauma. These middle meningeal artery fistulae demonstrated prominent orbital venous drainage through the sphenoparietal sinus and cavernous sinus in Case 6 and through the cavernous sinus in Case 5. These fistulae were treated by placing metallic coils transarterially in both patients. One patient (Case 5) also was embolized with PVA particles. Detachable balloons, metallic coils, PVA particles, silk suture, and liquid polymers can be used in the endovascular treatment of acquired arteriovenous fistulae. The embolic agent of choice depends upon the angiographic characteristics of the fistula.2,11
Direct and Indirect CCSFs
Although there are other techniques for treating direct and indirect CCSFs, placement of detachable balloons has been the mainstay of treatment for high-flow fistulae between the cavernous carotid artery and the cavernous sinus.2,11 Indirect CCSFs or dural arteriovenous fistulae usually require transarterial embolization of external carotid artery feeders, transvenous occlusion of the cavernous sinus, or both. Treatment includes various embolic agents such as metallic coils, silk suture, or even liquid adhesive agents.
Conclusions
A wide variety of vascular lesions may involve the orbit directly or indirectly. Improvements in microguidewire and microcatheter technology allow access to previously unreachable regions. The specific endovascular techniques used will vary according to the anatomy of the lesion. Treatment of these lesions often requires a multidisciplinary (surgery and/or radiation) approach to obtain the most satisfactory results. Superselective catheterization and embolization through the ophthalmic artery is now possible under the proper conditions. Placing the microcatheter distal to the central retinal artery and avoiding any reflux are important guidelines when embolization through the ophthalmic artery is being considered. Provocative testing with lidocaine should be used routinely before any anticipated ophthalmic artery embolization.4 If these recommendations and guidelines are followed, superselective embolization of orbital/periorbital AVMs and neoplasms through the ophthalmic artery may be undertaken with caution. The decision to proceed with this technique must follow a careful analysis of the risks and benefits as well as consideration of alternative methods of treatment. Direct puncture techniques can be performed safely in the orbit when the anatomic disposition of the lesion is favorable. Peri-orbital arteriovenous fistulae with abnormal orbital venous drainage can be treated effectively by transarterial and transvenous endovascular procedures. Meticulous angiographic workup and analysis in conjunction with interactive clinical consultation is necessary in planning the treatment of lesions that directly or indirectly involves the orbit.
References
- Berenstein A: Discussion of the treatment of capillary-venous malformations using a new fibrosing agent. Plast Reconstr Surg 71:613-614, 1983
- Dion J: Acquired cervicocranial arteriovenous fistulas. Neuroimaging Clin North Am 2:319-336, 1992
- Goldberg RA, Garcia GH, Duckwiler GR: Combined embolization and surgical treatment of arteriovenous malformation of the orbit.Am J Ophthalmol 116:17-25, 1993
- Horton JA, Dawson RC, III: Retinal Wada test. AJNR 9:1167-1168, 1988
- Lasjaunias P, Bernstein A: Surgical Neuro-Angiography. Berlin: Springer-Verlag, 1987
- Manelfe C, Lasjaunias P, Ruscalleda J: Preoperative embolization of intracranial meningiomas. AJNR 7:963-972, 1986
- Park K, Mannor GE, Wolfley DE: Preoperative embolization of an orbital brown tumor (letter). Am J Ophthalmol 117:679-680, 1994
- Riche MC, Hadjean E, Tran-Ba-Huy P, et al: The treatment of capillary-venous malformations using a new fibrosing agent. Plast Reconstr Surg 71:607-612, 1983
- Rootman J, Kao SC, Graeb DA: Multidisciplinary approaches to complicated vascular lesions of the orbit. Ophthalmology 99:1440-1446, 1992
- Tsai FY, Wadley D, Angle JF, et al: Superselective ophthalmic angiography for diagnostic and therapeutic use. AJNR 11:1203-1204, 1990
- Viñuela F, Halbach VV, Dion JE: Interventional Neuroradiology. Endovascular Therapy of the Central Nervous System. New York: Raven, 1992
