
Elongating a Bone Graft for Corpectomy: Technical Note
Mohammed A. Eleraky, MD
Jonathan J. Baskin, MD
Volker K. H. Sonntag, MD
Division of Neurological Surgery, Barrow Neurological Institute, St. Joseph’s Hospital and Medical Center, Phoenix, Arizona
Abstract
A patient who underwent a multilevel corpectomy for spondylitic myelopathy is presented. Intraoperatively, the large segment of autologous iliac crest graft harvested for reconstruction of the vertebral column was insufficient to span the required corpectomy defect. A novel method was devised to elongate the autologous bone graft. This technique salvaged the previously harvested bone graft, thereby avoiding the need to harvest a second, larger graft. The clinical and radiographic results appear to be comparable to those associated with the conventional grafting procedure.
Key Words : bone graft, cervical corpectomy, cervical fixation
After single or multiple-level discectomies or corpectomies are performed, the cervical spine can be reconstructed with allograft or autograft material. The graft and recipient site must be meticulously prepared to optimize the opportunity for arthrodesis (i.e., fusion) to occur. A critical factor for attaining osseous integration of the graft is placing it under compression between the two adjacent vertebral bodies. We describe a salvage technique that can be used to supplement an autograft that is found to be too small intraoperatively.1-4
Case Presentation
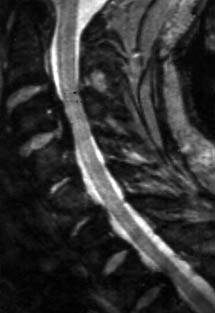
A 62-year-old male sought treatment for neck pain that radiated to the extremities, ataxia, dysphagia, urinary incontinence, fecal retention, and sexual dysfunction. Both magnetic resonance (MR) imaging and postmyelographic computed tomography (CT) demonstrated spinal cord compression secondary to ossification of the posterior longitudinal ligaments, which was most significant at the level of C3 and C4 (Fig. 1).
The patient underwent corpectomies of C3 and C4 to obtain adequate decompression of the spinal cord. The vertical extent of the corpectomy defect was measured, and a slightly longer autologous graft (45 mm) was harvested from the patient’s iliac crest. Unfortunately, further inspection of the operative site prompted additional undercutting of the adjacent surfaces of the C2 and C5 vertebral bodies. Consequently, the autograft was ultimately about 7 mm too short to span the corpectomy defect.
[one_third]
[/one_third]
[one_third]

[/one_third]
[one_third_last]

[/one_third_last]
Instead of harvesting a second, larger autologous iliac crest graft or using cadaveric allograft, a second, smaller piece of autologous bone (~1 cm) was harvested from the same graft site with the reciprocating saw. The two pieces of bone graft were then secured together with a titanium lag screw directed along the longitudinal axis of the bone. The patient’s head was gently distracted by the anesthesiologist, and the graft was tapped carefully within the corpectomy defect (Fig. 2).
An appropriately sized Atlantis plate (Sofamor-Danek, Memphis, TN) was placed from C2 to C5 (Fig. 3) and a screw used to secure the autograft to the plate.
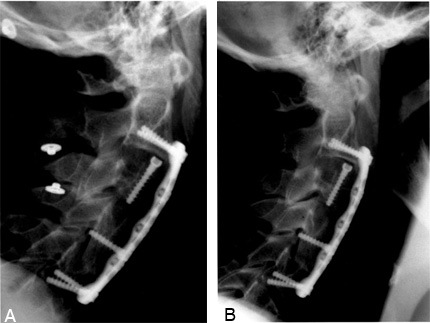
Postoperative MR imaging showed good decompression of the spinal cord. Neutral and dynamic cervical radio-graphs obtained 6 months after surgery showed the hardware to be in a stable position and evidence of fusion across both the graft-vertebral body and graft-graft interfaces (Fig. 4). Clinically, the patient’s preoperative myelopathy improved significantly.
Conclusion
We do not recommend deviating from the time-honored teaching of “measure twice, cut once.” However, the salvage procedure described here appears to have been successful in minimizing potential complications and expenses associated with miscalculating the necessary length of an autograft from the iliac crest.
References
- Awasthi D, Voorhies RM: Anterior cervical vertebrectomy and interbody fusion. Technical note. J Neurosurg 76:159-163, 1992
- Boni M: Stabilization of cervical spine: Problems and techniques. J Neurosurg Sci 28:167-171, 1984
- Kojima T, Waga S, Kubo Y, et al: Anterior cervical vertebrectomy and interbody fusion for multi-level spondylosis and ossification of the posterior longitudinal ligament. Neurosurgery 24:864-872, 1989
- Tew JM, Jr., Mayfield FH: Complications of surgery of the anterior cervical spine. Clin Neurosurg 23:424-434, 1976
