
Cerebellopontine Angle Glioblastoma Multiforme with Ventricular Metastases: Case Report
Cargill H. Alleyne, Jr., MD†
A. Giancarlo Vishteh, MD‡
Robert F. Spetzler, MD
Division of Neurological Surgery, Barrow Neurological Institute, St. Joseph’s Hospital and Medical Center, Phoenix, Arizona
Current Address: †Department of Neurosurgery, University of Rochester, Rochester, New York,
‡Quantum Neurological Surgery, Phoenix, Arizona
Abstract
Most lesions involving the cerebellopontine angle (CPA) are located extracranially and are acoustic schwannomas or meningiomas. Other less common lesions include epidermoid tumors, metastases, and arachnoid cysts. We report a lesion rarely found in the CPA. A 46-year-old man had a 4-week history of headaches and blurred vision. His imaging studies revealed a right CPA mass that appeared to be based on the petrous bone and metastases to the ependymal lining of the ventricles. The patient underwent subtotal resection of the lesion. The histology was consistent with glioblastoma multiforme (GBM). When a patient presents with a CPA tumor with evidence of ependymal spread, the diagnosis of GBM should be entertained.
Key Words: brain neoplasms, cerebellopontine angle, glioblastoma multiforme
Most lesions involving the cerebellopontine angle (CPA) are located extraaxially and are acoustic schwannomas or meningiomas. Other less common lesions include epidermoid tumors, metastases, and arachnoid cysts. Tumors that primarily involve the cerebellum, brain stem, or petrous bone can enter the CPA. Glioblastomas multiforme (GBMs) of the CPA are rare. We present a patient with a right CPA mass that appeared to be based on the petrous bone and showed evidence of metastases to the ependymal lining of the ventricles.
Case Report
A 46-year-old man with no significant medical history presented to another hospital after experiencing headaches and blurred vision for 4 weeks. A computed tomographic (CT) scan of the head showed an ill-defined mass in the right CPA. The patient was discharged and scheduled for an outpatient magnetic resonance (MR) imaging study of the brain. Two weeks later he presented to our institution with worsening headaches, nausea, vomiting, gait ataxia, and blurred vision.
On physical examination, he was well-developed, well-nourished and in no acute distress. He was afebrile and his vital signs were stable. On neurological examination, he was alert and fully oriented. His pupils were equally round and reacted to light. Bilateral sixth nerve palsies were present. There was mild ptosis of the left eye and dysfunction of the right seventh, eighth, ninth, tenth, and twelfth nerves. Finger-to-nose examination revealed dysmetria on the right. His right lower extremity was slightly weak and sensory testing was grossly normal.
A head CT scan without contrast showed the mass with obstructive hydrocephalus. The patient was admitted to the intensive care unit where a ventriculostomy was placed. Opening pressure was 16 cm of cerebrospinal fluid.
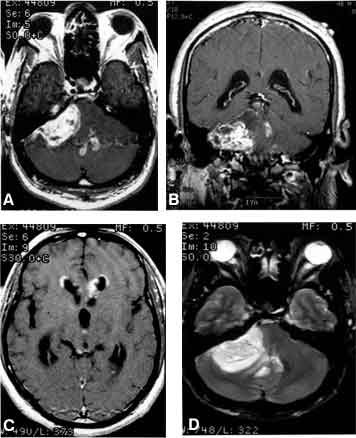
T1-weighted MR imaging confirmed the presence of a 4 x 3 cm CPA mass that compressed the fourth ventricle, causing obstructive hydrocephalus. Administration of gadolinium resulted in heterogeneous enhancement of the mass as well as enhancement of the ependymal surface of the fourth ventricle and of the frontal horns of the lateral ventricle. Perilesional edema was also present (Fig. 1).
The patient underwent a right posterior fossa craniotomy in the prone position. The tumor, which involved the cerebellar hemisphere (filling the CPA cistern), the seventh and eighth cranial nerves, and apparently the pons, was resected subtotally. Pathological examination of the specimen revealed cellular proliferation of atypical fibrillary astrocytes with mitotic figures and areas of arachnoid invasion. The presence of glial fibrillary acidic protein confirmed the glial origin of the neoplasm. Microvascular proliferation was consistent with a grade IV astrocytoma according to the classification system of the World Health Organization. The patient died 2 months after presentation.
Discussion
The location of the GBM in the CPA in this case is distinctly rare.1-8 Although direct extension of a GBM of the posterior fossa to the fourth ventricle has been noted,1,6 ependymal spread to the fourth and lateral ventricles as occurred in this case is unusual. Likewise, extracerebellar metastases have rarely been reported.2,4,7
In Dohrmann’s review of 33 cases of primary cerebellar GBMs, the male-to-female ratio was 2:1 with two-thirds occurring in adults.3 Their finding of these lesions in a predominantly lateral location (79%) contrasts with the midline location in eight of nine posterior fossa GBMs evaluated by MR imaging in a more recent study.6 Six of the latter cases were in the vermis and two were in the pons, but no CPA presentation was noted. The authors concluded that while differentiating a posterior fossa GBM from a metastatic tumor was difficult, the presence of heterogeneous and rim-like enhancement, a midline location, a poorly defined margin, tumoral hemorrhage, multicenter or multifocal lesions, and extra-axial or extracranial metastases might suggest the diagnosis of GBM. Our case emphasizes that when a patient presents with a CPA tumor with evidence of ependymal spread to the ventricles, the diagnosis of glioblastoma multiforme should be considered.
References
- Bhimani S, Virapongse C, Spencer D, et al: Case report. CT appearance of cerebellar glioblastoma multiforme. J Comput Assist Tomogr 7:889-891, 1983
- Chamberlain MC, Silver P, Levin VA: Poorly differentiated gliomas of the cerebellum. A study of 18 patients. Cancer 65:337-340, 1990
- Dohrmann GJ, Dunsmore RH: Glioblastoma multiforme of the cerebellum. Surg Neurol 3:219-223, 1975
- Hegedüs K, Molnár P: Primary cerebellar glioblastoma multiforme with an unusually long survival. Case report. J Neurosurg 58:589-592, 1983
- Kopelson G: Cerebellar glioblastoma. Cancer 50:308-311, 1982
- Kuroiwa T, Numaguchi Y, Rothman MI, et al: Posterior fossa glioblastoma multiforme: MR findings. AJNR 16:583-589, 1995
- Pang D, Ashmead JW: Extraneural metastasis of cerebellar glioblastoma multiforme. Neurosurgery 10:252-257, 1982
- Zito JL, Siva A, Smith TW, et al: Glioblastoma of the cerebellum. Computed tomographic and pathologic considerations. Surg Neurol 19:373-378, 1983
