
Assessment of Cervical Vascular Injury with CT Angiography
Patrick Fredenberg, MD
Kirsten Forbes, MD
Leon Toye, MD
Shahram Partovi, MD
Division of Neuroradiology, Barrow Neurological Institute, St. Joseph’s Hospital and Medical Center, Phoenix, Arizona
Abstract
Conventional digital subtraction angiography (DSA) is the diagnostic gold standard for cervical vascular injury following neck trauma. DSA, however, is invasive and thus inherently risky in unstable patients because of the arterial catheterization and the relatively lengthy examination. Recent advances in computed tomographic (CT) angiography have rendered this modality a potential alterative for investigating acute trauma. CT angiography is extremely rapid and minimally invasive, thus limiting the likelihood of complications. This article examines the role of CT angiography in the assessment of major and minor cervical vascular injury and compares its performance to that of DSA, magnetic resonance imaging, and ultrasonography.
Key Words: angiography, cervical vascular injury, computed tomography, neck trauma
The optimal means of evaluating patients with neck trauma for cervical vascular injury remain controversial. A clinical assessment can identify patients with a high likelihood of vascular injury, but a negative examination provides little reassurance.[23] Approximately a third of subjects with a penetrating neck injury will have an associated vascular injury, many of whom will be asymptomatic initially.[10] There is a clear role for screening such patients for arterial damage. Cerebral angiography remains the gold standard technique for vascular imaging but is associated with inherent risks and therefore may not be the ideal screening procedure in this situation.[7] This article compares computed tomography (CT) angiography as a technique for detecting posttraumatic cervical vascular injury with both conventional angiography and other noninvasive imaging modalities.
Vascular Injury After Neck Trauma
Injury to the cervical arteries is not only more common after penetrating neck trauma but also is associated with a higher mortality rate (22%) than blunt injury (7%).[1,18] Of vascular injuries caused by penetrating trauma, 80% involve the carotid arteries. Injury to the internal carotid arteries (ICAs) is associated with higher morbidity and mortality rates than injuries to the common carotid artery.[11,18] The vertebral artery is less likely to be affected by penetrating trauma because it is smaller and deeper than the carotid arteries. Nonetheless, gunshot wounds involving the posterior neck can injure the vertebral artery by the widespread deposition of shrapnel.
Nonpenetrating trauma of the neck is a much less common cause of cervical vascular injury. It occurs in less than 1% of cases and tends to involve the vertebral artery rather than the carotid artery.[6] Most injuries result from hyperflexion, extension, or rotation, often from motor vehicle accidents[12] or infrequently from chiropractic manipulation of the neck.[21] Sometimes no definable event precedes the injury. In such cases, the patient should be evaluated fully for a predisposing vasculopathy such as fibromuscular dysplasia or a connective tissue disease. The low incidence of vascular injury after blunt neck trauma supports selective screening of patients with noninvasive imaging modalities. Patients with fractures involving the carotid canal or vertebral foramen warrant more aggressive vascular screening. Such fractures injure the ICA in 20% of the cases[19] and the vertebral artery in 46%. Facet dislocations carry an even higher risk of vascular injury.[25]
Traumatic effects on the artery depend on the extent and location of damage to the vessel wall.[14] Disruption of the intima can lead to subintimal dissection, which is more often associated with blunt than penetrating trauma.[18] Loss of intimal integrity, typically from a penetrating injury, predisposes patients to thrombosis, which can cause vascular stenosis, occlusion, or distal embolism.[9]
Pseudoaneurysms develop after the adventitia has been damaged and should be distinguished from true aneurysms affecting the media. Pseudoaneurysms are particularly common after penetrating injuries to the neck and account for about a third of ICA lesions.[9] With blunt trauma, pseudoaneurysms are rare and the associated mortality rate is low.[2] Penetrating trauma also can lead to complete arterial transection or to the formation of an arteriovenous (AV) fistula.[1]
Diagnostic Imaging of Cervical Vascular Injuries
The imaging assessment of cervical arteries should determine both the site and nature of an injury and the adequacy of collateral circulation.[20] Both intra- and extracranial vessels should be examined, including the origins of major vessels. Repeated imaging also may be beneficial, particularly given the potential for delayed development of an aneurysm or fistula after trauma.[3]
The gold standard for imaging cervical vascular injury is contrast angiography. This technique offers high spatial resolution, which allows subtle radiographic abnormalities such as intimal flaps or arterial tapering to be detected. The artery can be evaluated for a predisposing arteriopathy such as fibromuscular dysplasia, which also can underlie vascular injury. If a traumatic aneurysm or AV fistula is present, diagnostic angiography can be combined with endovascular treatment such as coiling. However, the relatively long duration of digital subtraction angiography (DSA) in an often unstable patient remains a concern. Patients have a higher risk of developing ischemic symptoms during the procedure than the 0.5 to 1% risk of stroke observed in the general population. Therefore, this technique is not ideal for screening.[8]
Ultrasonography
Ultrasonography provides a safe, quick, and noninvasive assessment of the cervical arteries, and several centers have reported that its sensitivity to posttraumatic findings is high.[4,5,13] Ultrasonography, however, also has significant limitations. In the setting of neck trauma, accurate evaluation may be limited by subcutaneous air or an echogenic hematoma overlying the vessel of interest. The distal ICA above the angle of the mandible (zone III) and its more proximal segment under the clavicle (zone I) cannot be evaluated directly. Ultrasonographic evaluation of aneurysms or AV fistulae is limited as is assessment of underlying vasculopathy. Finally, ultrasonography is highly operator dependent.
Magnetic Resonance Imaging
Magnetic resonance (MR) imaging offers an alternative examination for evaluating vascular sequelae after neck trauma.[24] Both MR angiography and fat-saturated T1-weighted axial images are useful tools for assessing dissection of cervical vessels. These techniques, however, are insensitive to small intimal flaps. Fat-saturated axial T1-weighted images allow detection of high-intensity signals from subacute thrombus within the vessel wall. They are less sensitive to acute thrombus because its signal is isointense. It is difficult to separate partial from complete vessel occlusion with MR angiography because it detects slow blood flow poorly. Small pseudoaneurysms also can be missed.
MR imaging is superior to CT in that it provides additional information about the soft tissues of the neck. Consequently, spinal cord injury, epidural hematomas, and ligamentous or disc disease can be detected. Diffusion-weighted imaging allows the brain to be assessed for ischemic damage after a cervical vascular injury. In the setting of acute trauma, however, MR imaging is unsuitable for patients with gunshot injuries when shrapnel lies close to vital structures. Shrapnel also causes considerable artifact because it is metallic and signals can drop out. The long imaging times associated with MR imaging also are suboptimal in unstable patients when opportunities for patient monitoring are limited. Furthermore, special equipment such as nonmagnetic pumps is required for use with MR imaging.
CT Angiography
CT angiography offers a rapid, minimally invasive assessment of the cervical arteries. This technique has benefited markedly from the development of both spiral CT and, more recently, multidetector capabilities. These hardware improvements have significantly reduced scanning time, enabling imaging to be performed during maximal arterial opacification. The intravenous mode of delivery of iodinated contrast is associated with significantly fewer procedural complications than conventional intra-arterial contrast angiography. This technique easily can be added to routine imaging of the cervical spine, offering a screening tool for vascular injury from either penetrating[15] or blunt[22] trauma. Additional scanning time is minimal (less than 30 seconds). Thus, patient monitoring is uncompromised and treatment is not delayed. Furthermore, the minimally invasive nature of the technique allows repeated follow-up imaging as necessary.

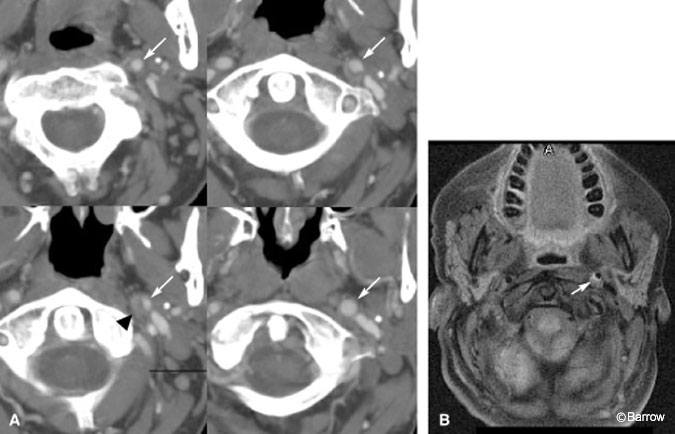
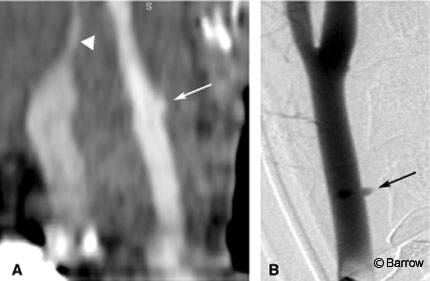
right common carotid artery (arrow), consistent with a small pseudoaneurysm, in a 28-year-old male with a stab wound to the neck. An associated neck hematoma compresses the jugular vein (arrowhead). (B) Lateral digital subtraction angiogram confirms the presence of the pseudoaneurysm (arrow).
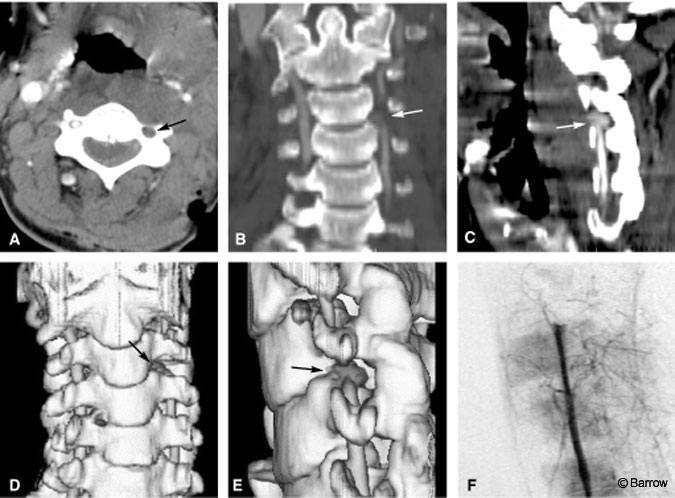
The current use of CT angiography for assessing a cervical arterial injury is limited, and its true accuracy remains to be fully determined. In a number of small series,[15-17,22] the sensitivity and specificity of CT angiography to dissections, occlusions, pseudoaneurysms, and fistulae have been high. CT angiography reveals findings similar to those of conventional angiography, including contrast extravasation (Fig. 1), vessel occlusions (Fig. 2), acute dissections (Fig. 3), intimal flaps (see CT Angiography and Stroke in this issue), and pseudoaneurysms (Fig. 4). It also provides additional information about surrounding soft tissues. There is concern that CT angiography may miss small intimal flaps or dissections.[10] Such patients, however, often exhibit indirect evidence of injury, for example, bone and bullet fragments less than 5 mm from a major vessel, the path of injury extending through a vessel, and adjacent hematoma.[10] These findings should prompt assessment with conventional angiography.
CT angiography offers additional benefit compared to ultrasonography in that it directly visualizes the ICA within the skull base. It offers better visualization of the origins of major vessels than ultrasonography, but its accuracy in detecting injuries in zone I may be limited by streak artifacts from the shoulders. Bullet fragments also can cause streak artifact that can obscure underlying vessels and necessitate conventional angiography.
Conclusion
Multidetector CT angiography offers a quick and minimally invasive technique for evaluating the cervical arteries of patients with neck trauma. We have used CT angiography to identify vascular lacerations and contrast extravasation, occlusions, and dissections in both the cervical carotid and vertebral arteries. DSA remains the diagnostic gold standard but should be used to exclude a lesion when CT angiography is negative but clinical suspicion is high. When a traumatic vascular injury is visualized on CT angiography, the need for purely diagnostic DSA is questionable. Given its relative noninvasiveness, CT angiography also may be used to follow patients who have been treated for a traumatic vascular injury.
References
- Brown MF, Graham JM, Feliciano DV, et al: Carotid artery injuries. Am J Surg 144:748-753, 1982
- Cogbill TH, Moore EE, Meissner M, et al: The spectrum of blunt injury to the carotid artery: A multicenter perspective. J Trauma 37:473-479, 1994
- Fabian TC, George SM, Jr., Croce MA, et al: Carotid artery trauma: Management based on mechanism of injury. J Trauma 30:953-961, 1990
- Fry WR, Dort JA, Smith RS, et al: Duplex scanning replaces arteriography and operative exploration in the diagnosis of potential cervical vascular injury. Am J Surg 168:693-695, 1994
- Ginzburg E, Montalvo BM, LeBlang SD, et al: The use of duplex ultrasonography in penetrating neck trauma. Arch Surg 131:691-693, 1996
- Golueke P, Sclafani S, Phillips T, et al: Vertebral artery injury–diagnosis and management. J Trauma 27:856-865, 1987
- Heiserman JE, Dean BL, Hodak JA, et al: Neurologic complications of cerebral angiography. AJNR Am J Neuroradiol 15:1401-1411, 1994
- Katirji MB, Reinmuth OM, Latchaw RE: Stroke due to vertebral artery injury. Arch Neurol 42:242-248, 1985
- Kuehne JP, Weaver FA, Papanicolaou G, et al: Penetrating trauma of the internal carotid artery. Arch Surg 131:942-947, 1996
- LeBlang SD, Nunez DB, Jr.: Noninvasive imaging of cervical vascular injuries. AJR Am J Roentgenol 174:1269-1278, 2000
- Meier DE, Brink BE, Fry WJ: Vertebral artery trauma: Acute recognition and treatment. Arch Surg 116:236-239, 1981
- Moar JJ: Traumatic rupture of the cervical carotid arteries: An autopsy and histopathological study of 200 cases. Forensic Sci Int 34:227-244, 1987
- Montalvo BM, LeBlang SD, Nunez DB, Jr., et al: Color Doppler sonography in penetrating injuries of the neck. AJNR Am J Neuroradiol 17:943-951, 1996
- Morgan MK, Besser M, Johnston I, et al: Intracranial carotid artery injury in closed head trauma. J Neurosurg 66:192-197, 1987
- Munera F, Soto JA, Palacio D, et al: Diagnosis of arterial injuries caused by penetrating trauma to the neck: Comparison of helical CT angiography and conventional angiography. Radiology 216:356-362, 2000
- Ofer A, Nitecki SS, Braun J, et al: CT angiography of the carotid arteries in trauma to the neck. Eur J Vasc Endovasc Surg 21:401-407, 2001
- Prokesch RW, Goerzer HF, Killer M, et al: Pseudoaneurysm of the internal carotid artery after shrapnel injury in World War II: Demonstration by CT angiography with 3D MIP reconstruction. Eur Radiol 9:1441-1444, 1999
- Ramadan F, Rutledge R, Oller D, et al: Carotid artery trauma: A review of contemporary trauma center experiences. J Vasc Surg 21:46-55, 1995
- Resnick DK, Subach BR, Marion DW: The significance of carotid canal involvement in basilar cranial fracture. Neurosurgery 40:1177-1181, 1997
- Richardson JD, Simpson C, Miller FB: Management of carotid artery trauma. Surgery 104:673-680, 1988
- Robertson JT: Neck manipulation as a cause of stroke (editorial). Stroke 12:1, 1981
- Rogers FB, Baker EF, Osler TM, et al: Computed tomographic angiography as a screening modality for blunt cervical arterial injuries: Preliminary results. J Trauma 46:380-385, 1999
- Sclafani SJ, Cavaliere G, Atweh N, et al: The role of angiography in penetrating neck trauma. J Trauma 31:557-562, 1991
- Weller SJ, Rossitch E, Jr., Malek AM: Detection of vertebral artery injury after cervical spine trauma using magnetic resonance angiography. J Trauma 46:660-666, 1999
- Willis BK, Greiner F, Orrison WW, et al: The incidence of vertebral artery injury after midcervical spine fracture or subluxation. Neurosurgery 34(3):435-441, 1994
