
Feasibility of a Resorbable Anterior Cervical Graft Containment Plate†
Authors
Christopher P. Ames, MD‡
Robert H. Chamberlain, BSE
G. Bryan Cornwall, PhD*
Neil R. Crawford, PhD
Eric W. Nottmeier, MD§
Volker K. H. Sonntag, MD
Spinal Biomechanics Research Laboratory, Division of Neurological Surgery, Barrow Neurological Institute, Phoenix, Arizona and *MacroPore Biosurgery, San Diego, California
Current Addresses:
‡Department of Neurosurgery, UCSF, San Francisco, California
§Department of Neurosurgery, Mayo Clinic, Jacksonville, Florida
†This article is modified from Ames et al: Feasibility of a resorbable anterior cervical graft containment plate. Orthopedics Supplement 25(10):1-7, 2002. With permission from SLACK, Incorporated.
Abstract
This article reviews the background of anterior cervical plating for one- and two-level diskectomy for degenerative disease and justifies the design and testing of a cervical plate composed of a resorbable material. Special consideration is given to modifications of implant design and related implant tools because these less rigid materials have different mechanical properties compared to metallic plates. Our cadaveric and animal in vivo testing methodologies, a novel testing method that reliably quantifies graft containment, and data from a representative sample are presented. The advantages and disadvantages of resorbable plating are also discussed.
Key Words: biomechanical testing, cervical spine, diskectomy, resorbable implants
Most single-level plates are placed during anterior cervical diskectomies for the treatment of herniated cervical disks and foraminal stenosis associated with disk-osteophyte complexes.[7,9] In these cases the posterior stabilizers of the cervical spine are usually intact, and the flexion-resistance stress placed on the cervical plate is not extensive. A cervical plate made of a nonmetallic material that would be fully compatible with magnetic resonance (MR) imaging, less stiff than titanium (possibly decreasing the incidence of adjacent segment disease), and resorbable would have many advantages compared to metallic plates. Such a device would eliminate adverse effects on spinal biomechanics and the possibility of late hardware-related complications associated with rigid plates once the stabilizing function is no longer required.
For several years, resorbable polylactide polymers have been used in numerous human clinical applications, particularly craniofacial fixation.[4,8] The authors conducted initial biomechanical testing in a cadaveric diskectomy model of a prototype graft-containment mesh composed of 70/30 D,L-PLa. This article describes the implant and basic testing methodology.

Implant Description
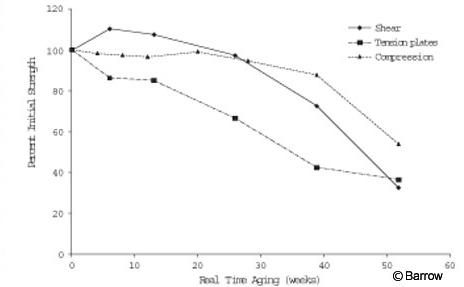
The implant resembles a craniofacial mesh with partially recessed screw holes, but the design is thicker (1.6 mm) and has wider spacing between the holes (Fig. 1). The resorbable mesh is available in various sizes and is composed of 70/30 poly(L-lactide-co-D,L-lactide) (70/30 D,L-PLa; MacroPore Biosurgery Inc., San Diego, CA). The polylactide polymer is degraded in vivo through hydrolysis to lactic acid, a natural byproduct of anaerobic metabolism. The process of hydrolysis involves a gradual change in the strength of the implant material. At 6 months, the polymer has about 90% of its original strength and at 9 months about 70% of its original strength (Fig. 2). The implant dimensions can be modified to increase its thickness. This feature may provide sufficient strength for a graft-containment function in the cervical spine.
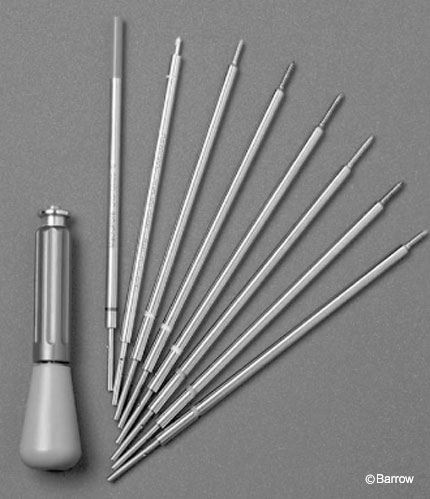
The instrumentation set consists of an awl, hand drill, tap, and screwdriver, all of which require a single handle (Fig. 3). The hole size and tap are designed specifically to permit the plate to be threaded during the tapping process.

Threading increases the strength of the screw-plate interface, thus decreasing the risk of screw backout. Threading also creates some resistance to the screw toggling at the plate interface. The plate can then function as a cantilever for added stability.
The screw head incorporates a special design to distribute the torsional forces evenly around the circumference of the head to facilitate screw insertion (Fig. 4). This design is necessary because the material is less rigid than metal. In addition, the end of the screwdriver has a patented design intended to engage with the surface of the plate and to eject the screwdriver tip once the screw has been tightened.
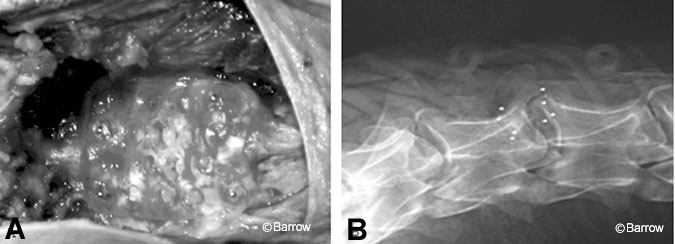
This design prevents the screw head (2.7 mm x 12 mm) from stripping. For in vivo analysis, radiopaque tantalum marker beads were incorporated into the head and tip of the screws and into the ends of the plate. Beads of 1-mm diameter were used in the head and tip of the screw, and 0.5-mm beads were used in the plate to facilitate their radiographic differentiation. Tantalum is an approved biomaterial (ASTM F560-96).

Implant Insertion
The single-level plate was affixed to the spine after the graft was placed with four to six screws (2.7 mm x 12 mm). Two to three screws were inserted at each level (Fig. 5A). First, prominent anterior osteophytes were removed. The plate was then soaked in a preheated water bath at 65º C to facilitate contouring. The water bath heats the polymer above the glass transition temperature and allows it to be formed with standard surgical tools.
Once the implant has cooled to room or body temperature, it becomes rigid and maintains the newly contoured shape without loss of its original mechanical properties. The plate was contoured to sit as flush as possible to the anterior surface of the spine. This maneuver usually involved creating a mild lordosis and tubular curvature (Fig. 5B).
A round-handled instrument, such as the handle of a curette, was used to help create the smooth tubular contour. When two screws were inserted, the most lateral holes at the superior aspect of the plate were used. When three screws were used, the second hole in the superior aspect of the plate was also used (Fig. 1).
Experimental Design
To achieve the most clinically applicable comparison, a human cadaveric one- and two-level diskectomy model was tested in 20 specimens (Table 1). Distraction and endplate preparation were performed the same in all specimens.
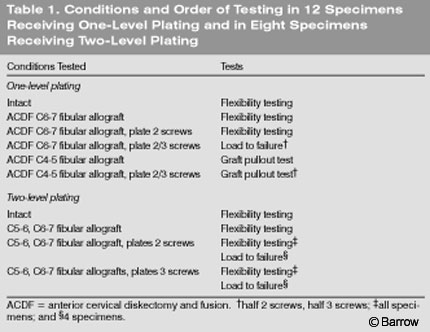
A Cornerstone-SR cutter and interspace sizers (Medtronic Sofamor Danek, Memphis, TN) were used to standardize the size of the graft and the compression (interbody distraction) forces applied to it. In the two-level models, a longer plate was used and screws were placed in the intervening vertebral body. Load to failure was tested during flexion, which is the weakest loading modality for anterior cervical plates.

Flexibility and Load-to-Failure Testing
Nonconstraining, nondestructive pure-moment loading was applied to each specimen through a system of cables and pulleys in conjunction with a standard servohydraulic test system (MTS, Minneapolis, MN; Fig. 6).[5] Three cycles of preconditioning were used. Loads were applied about the appropriate anatomical axes to induce three different types of motion: flexion-extension, lateral bending, and axial rotation. Three-dimensional specimen motion in response to the loads was determined using the Optotrak 3020 system (Northern Digital, Waterloo, Ontario, Canada). This system stereophotogrammetrically measures the three-dimensional displacement of infrared-emitting markers rigidly attached in a noncollinear arrangement to each vertebra. Custom software converted the marker coordinates to angles about each of the anatomical axes. Specimens were loaded quasistatically to a maximum of 1.5 Nm.
Immediately after flexibility testing, most specimens were loaded to failure (Table 1). During flexion, specimens were loaded at a constant displacement rate of 1º/second until failure was visible. Applied load was monitored from the load cell attached to the cables and pulleys as well as from the six-axis load cell located below the vise that anchors the specimen. Data from the load cells were recorded at 2 Hz.

Graft-Containment Testing
Currently, no technique is accepted as the standard for testing the effectiveness of a plate in preventing graft extrusion. Graft containment was therefore quantified as follows. A metallic chain was placed posterior to the graft and connected anteriorly to a uniaxial load cell in series with the piston of the MTS unit. The specimen was secured to a fixed support at both ends. The chain was positioned so that it did not directly contact the plate. The chain was slowly advanced in a posterior-to-anterior direction at a rate of 5 mm/min until extrusion or gross failure of the graft was visible (Fig. 7).
Tension on the chain primarily produced a shear force on the graft and plate and secondarily an extension moment at the graft site. This failure mode correlates well with clinical failure because extension of the neck is the mode most likely to cause graft extrusion.[4,5] Load and displacement were recorded continuously at 2 Hz. Visible extrusion was defined as migration of the anterior aspect of the allograft 0.5 mm beyond the anterior aspect of the vertebral body. Gross failure was defined as significant graft fracture or fragmentation such that support of the anterior column was lost. The endplates were inspected after each test, but no damage was detected. Had endplate damage been detected, the specimens would have been divided into two groups: half without a plate and half with a plate. The allograft was also inspected. If damage was detected, a new allograft of identical size was used for the second stage of pullout testing at that level.
Results
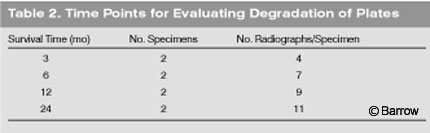
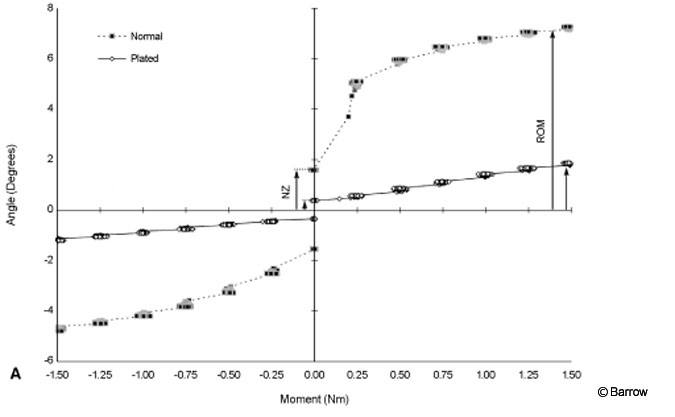
Biomechanical test results are under analysis. The results will be compared with in vivo data from a simultaneous animal study using a sheep anterior cervical diskectomy autograft model at C3-C4 (unpublished data). Plots of angular deformation as a function of load allowed motion in normal and plated specimens to be compared (Fig. 8A). Plots of pullout force as a function of linear deformation allowed pullout resistance to be compared in plated and unplated specimens (Fig. 8B). These single specimen graphs were selected at random to illustrate data collection methods. As samples of data, they should not be interpreted as representative of the as of yet unpublished comprehensive biomechanical analysis. The in vivo portion of the analysis requires several time points to evaluate degradation of the plate (Table 2). Thus far, two specimens from the 3-month time point from the in vivo sheep portion of the study have been evaluated. At that time, the structural integrity of the plate was well maintained and the small radiopaque markers were well visualized on standard radiography. Flexibility testing showed significant rigidity of the plated segment compared to adjacent levels (Fig. 9).
Discussion
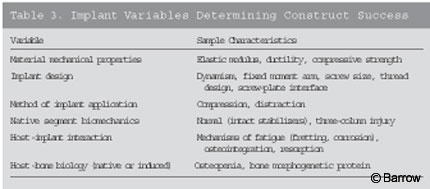
The minimum mechanical characteristics for a specific material to function effectively as a plate, to increase fusion rates above those of bone graft alone, and to prevent complications such as graft dislodgement when anterior cervical diskectomy is indicated are unknown. Most likely, the implant must create and maintain a minimum amount of rigidity across the segment to allow arthrodesis. A minimal amount of load sharing with the graft must be maintained and a minimal amount of time must elapse for the fusion to develop. These properties are a function of the mechanical properties of the implant material, the design elements of the implant, the way in which the implant is applied, the preexisting biomechanical properties of the cervical segment, characteristics of the implant-host reaction, and native and induced biology of the host bone (Table 3).
Fixation and Fusion
Biomechanical studies have demonstrated that anterior cervical plates offer additional stability compared with bone grafts alone.[6] The risk-benefit ratio of adding an anterior plate to a single-level diskectomy and fusion is controversial because the rate of uninstrumented fusion in this region is high.[1] In a recent report, however, the addition of anterior cervical plating to a single-level anterior cervical diskectomy increased fusion rates from 90% to 96%.[7,9,11] Furthermore, no clinically significant complications were related to the instrumentation in the group that received plates. Graft-related complications also decreased significantly in the instrumented cohort.
The pseudarthrosis rates associated with multilevel anterior cervical diskectomies are significantly higher in patients treated without plate fixation. For two-level anterior cervical diskectomies without plating, pseudarthrosis rates ranged from 25% to 28% in a large series.[9] In contrast, the addition of plating to a two-level diskectomy with autograft has reduced the failure rate of fusion.[10]
During the past decade, particularly after the development of the current generation of cervical locking plates, the use of instrumentation with a single-level diskectomy increased dramatically. The advantages of an anterior cervical screw plate include its mechanical effect for providing internal fixation and for reducing the postoperative need for external cervical orthoses. In the senior author’s (VKHS) practice during the past 2 years, more than 100 single-level anterior cervical diskectomies have been performed to treat disk herniations and degenerative disease. All nonsmoking patients who require single-level diskectomy were offered the choice of instrumented fusion with no postoperative bracing or uninstrumented fusion with 6 weeks of cervical bracing. Every patient elected placement of a cervical plate. Consequently, the plating procedure has become the senior author’s standard procedure. Furthermore, almost all patients are offered the choice between allograft and autograft bone. In the past year, only one patient has chosen autograft.
Mechanically, anterior cervical screw plates function as a tension band and a buttress plate. These devices resist cervical extension, axial rotation, and lateral bending relatively efficiently. Anterior cervical screw plates are weakest in resisting neck flexion, particularly if the posterior elements of the cervical spine have been disrupted (i.e., by postlaminectomy, facet fractures, hyperflexion injuries with ligament tears). The extent of fixation depends on bone mineral density. Dense bone provides a strong anchor for the screws. Osteoporotic bone holds screws poorly. Cervical screw plates can act to prevent movement of unstable vertebrae, to prevent graft extrusion or displacement, and to maintain compression of graft materials.
Disadvantages of Metallic Plates
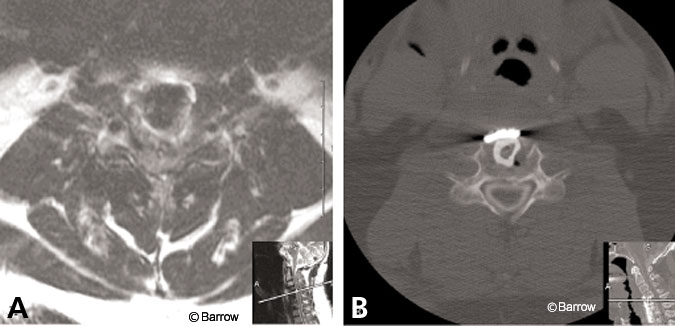
Most cervical plates are composed of titanium alloys, the most popular of which is Ti-6Al-4V. These plates provide significant rigidity across the fused segment and typically are associated with low rates of hardware-related complications such as infection, fracture, and screw backout. On magnetic resonance (MR) imaging, titanium produces substantial artifact that may make postoperative imaging difficult to interpret at the instrumented levels. If imaging is needed, computed tomography (CT)-myelography is required to assess the spinal canal accurately after a titanium plate has been implanted (Fig. 10).
It has been postulated that the addition of a plate may increase the incidence of degenerative disease at adjacent segments. The underlying mechanism has been attributed to increased dissection of the anterior longitudinal ligament near the adjacent levels.[7] Possibly, the high rigidity conferred on the fusion segment by the addition of a stiff titanium plate may contribute to the development of adjacent segment degenerative disease, particularly if the ends of the plate are near the adjacent levels.
Another disadvantage associated with metallic plates is the difficulty in visualizing the bone during insertion caused by the plate’s opacity. Furthermore, the implant persists beyond the time required for fusion to occur.
Features of Resorbable Plates
Whether cervical screw plates predispose patients to stress shielding or accelerated degeneration of motion segments adjacent to the fused spine is unclear. These effects are believed to be decreased with dynamic variable-angle screw plates that enable greater load sharing in the setting of normal subsidence.[2] The resorbable polymer plate provides dynamic load sharing in two ways. First, the threaded screw-plate interface formed by the process of tapping the plate hole allows some dynamic toggling of the screw much like the variable angle Atlantis plate but with less initial rigidity. Second, the resorption process slowly weakens the material. The rigidity of the plate (anterior tension band forces) and screw-plate interface (cantilever forces) further decreases with time. The design allows acute subsidence via screw toggling and chronic subsidence via resorption-induced weakening of the material.
It is unlikely that the PLA polymer plate will be as rigid as metallic plates in all loading modes. For one-level diskectomies performed for degenerative disease, however, significant hardware rigidity may be unnecessary or even undesirable. A less rigid construct such as the resorbable plate, which still provides a buttress effect and moderately increases the rigidity of the construct, may be all that is required to achieve the small (6%) reported increase in fusion rates compared to allograft alone.[7] Even if the resorbable plate does not increase fusion rates compared to allograft and external orthosis alone, patients may still prefer the resorbable construct if it spares them the 6-week period of relative immobility and inability to drive. In this case, the plate may be thought of as a temporary internal orthosis. It was specifically designed to be used for anterior cervical diskectomies performed to treat degenerative indications that leave the natural stabilizers of the posterior column intact.
Conclusion
MacroPore material and the design described here could offer several potential advantages for certain indications compared to available metallic plates.[10] The nonmetallic nature of the material offers an important advantage for postoperative imaging. The relative translucency also may increase the ease and accuracy of insertion. The specific clinical advantages or disadvantages of the property of resorbability are still unclear. Large randomized prospective trials are necessary to determine whether adjacent segment degeneration or the late failure of hardware is reduced by the use of resorbable polymer implants.
References
- Branch CL, Jr: Anterior cervical fusion: The case for fusion without plating. Clin Neurosurg 45:22-24, 1999
- Brodke DS, Gollogly S, Alexander Mohr R, et al: Dynamic cervical plates: Biomechanical evaluation of load sharing and stiffness. Spine 26:1324-1329, 2001
- Cauthen JC, Kinard RE, Vogler JB, et al: Outcome analysis of noninstrumented anterior cervical discectomy and interbody fusion in 348 patients. Spine 23:188-192, 1998
- Cohen SR, Holmes RE: Internal Le Fort III distraction with biodegradable devices. J Craniofac Surg 12:264-272, 2001
- Crawford NR, Brantley AG, Dickman CA, et al: An apparatus for applying pure nonconstraining moments to spine segments in vitro. Spine 20:2097-2100, 1995
- Grubb MR, Currier BL, Shih JS, et al: Biomechanical evaluation of anterior cervical spine stabilization. Spine 23:886-892, 1998
- Kaiser MG, Haid RW, Jr, Subach BR, et al: Anterior cervical plating enhances arthrodesis after discectomy and fusion with cortical allograft. Neurosurgery 50:229-238, 2002
- Kaptain GJ, Vincent DA, Laws ER, Jr: Cranial base reconstruction after transsphenoidal surgery with bioabsorbable implants. Neurosurgery 48:232-234, 2001
- Martin GJ, Jr, Haid RW, Jr, MacMillan M, et al: Anterior cervical discectomy with freeze-dried fibula allograft. Overview of 317 cases and literature review. Spine 24:852-859, 1999
- Wang JC, McDonough PW, Endow K, et al: The effect of cervical plating on single-level anterior cervical discectomy and fusion. J Spinal Disord 12:467-471, 1999
- Wang JC, McDonough PW, Endow KK, et al: Increased fusion rates with cervical plating for two-level anterior cervical discectomy and fusion. Spine 25:41-45, 2000
