
Herniated Lumbar Disk Sequestered Between the Internal and External Dural Sleeves: Case Report
Authors
Jeff Klopfenstein, MD
Patrick P. Han, MD
Louis Kim, MD
Robert F. Spetzler, MD
Division of Neurological Surgery, Barrow Neurological Institute, St. Joseph’s Hospital and Medical Center, Phoenix, Arizona
Abstract
Intradural lumbar disk herniation is common, but we report the first case of a herniated lumbar disk sequestered between the internal and external dural sleeves. A 50-year-old man sought treatment after 5 months of severe upper lumbar pain radiating into the proximal left lower extremity. Magnetic resonance imaging revealed a 3.0 x 1.5 x 1.5 cm, homogeneously enhancing mass in the left lateral recess of L1. The imaging characteristics were thought to be consistent with an intradural extramedullary neoplastic process. The patient underwent an L1 laminectomy. Exploration revealed a large fragment of disk material located between the inner and outer layers of the dura. The lesion was excised and sent for histopathologic examination. Final pathological analysis confirmed the diagnosis of nucleus pulposus. Surgeons should be aware of the possibility of a disk fragment sequestered between the internal and external dural sleeves when imaging studies suggest an intradural extramedullary neoplasm.
Key Words: disk herniation, dural sleeves, intradural
Intervertebral disk herniation is one of the most common entities treated by neurosurgeons. A rare variation of this condition occurs when all or part of the herniated disk material is located intradurally. Although relatively uncommon, intradural disk herniation is well documented. Walter Dandy first published such a case in 1942.[4] Since then more than 100 cases spanning the cervical, thoracic, and lumbar regions have been reported. To date, however, in all published cases of intradural disk herniation the disk material has been entirely intradural. We present a patient with a lumbar disk herniation contained entirely between the inner and outer dural sleeves.
Case Report
A 50-year-old man sought treatment after 5 months of severe, unrelenting upper lumbar pain with intermittent radiation into the left thigh. He reported ongoing paresthesias in the same distribution. The onset of his symptoms occurred acutely after bending over and was described as a “tremendous, sharp pain.” He denied subjective weakness or changes in bowel or bladder functions. Initially, the patient sought chiropractic treatment, which provided no benefit. Subsequently, he was referred for neurological evaluation through his primary care physician.
Examination
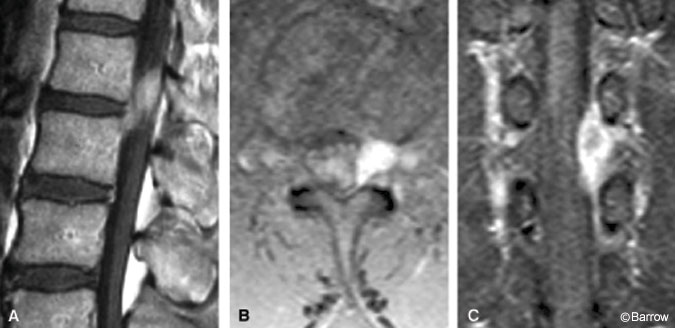
The patient’s general and neurological examinations were normal. Magnetic resonance (MR) images of the lumbar spine with and without gadolinium (Fig. 1) revealed a 3.0×1.5×1.5 cm, homogeneously enhancing lesion within the left lateral recess of L1 and neural foramen with no obvious connection to the disk space. The lesion was isointense to muscle on noncontrasted T1-weighted images. Based on the MR imaging findings, the lesion was thought to represent an intradural mass associated with the nerve root, most likely a schwannoma or neurofibroma. Less likely but also considered in the differential diagnosis were lymphoma, meningioma, metastasis, and herniated disk.
Surgical Procedure
The patient was positioned prone on the Wilson frame. An L1 en bloc laminectomy was performed with the intent to perform laminoplasty after the lesion was resected. Under microscopic visualization, the dura was opened sharply and intradural exploration was performed. No obvious lesion was identified. Attention was shifted to the external surface of the dura, and a prominent bulge was identified on the left anterolateral aspect of the thecal sac.
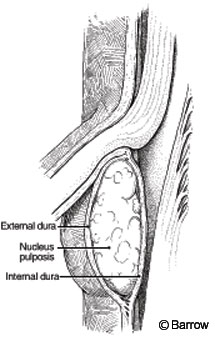
Sharp dissection was again used to incise the outer layer of the dura overlying the dural prominence. Immediately apparent was a yellowish-white, spongy mass lying superficial to the internal dural sleeve (Fig. 2). The mass was teased from between the inner and outer dural layers and sent for histopathologic examination. The inner dural layer remained intact. A watertight dural closure was obtained using 6-0 Prolene (Ethicon, Somerville, NJ) in a running fashion. The posterior elements were reapproximated using titanium miniplates, and a multilayer soft-tissue closure concluded the case.
Histopathology
Microscopic examination of the hematoxylin and eosin-stained sample revealed the presence of physaliphorous cells scattered in irregular clumps in a predominant background of extracellular matrix. The material was thought to be consistent with nucleus pulposus, confirming the diagnosis of herniated disk.
Histopathology
Microscopic examination of the hematoxylin and eosin-stained sample revealed the presence of physaliphorous cells scattered in irregular clumps in a predominant background of extracellular matrix. The material was thought to be consistent with nucleus pulposus, confirming the diagnosis of herniated disk.
Postoperative Course
Upon waking in the recovery room, the patient reported complete resolution of his thigh pain. He remained hospitalized for 2 days during which he was progressively mobilized. At discharge the patient was neurologically intact, and his only complaint was incisional pain. At early follow-up, the patient had continued to improve and had no neurological deficits.
Discussion
Based on their literature review as of 1994, Reina et al. reported 79 published cases of intradural disk herniations.[14] Included among these was Dandy’s original report in 1942.[4] Since 1994 an additional 25 cases have been published,[1-3,5,6,9-13,15,17] for a total of 104 reported lumbar intradural disk herniations as of 2002. None of the reported cases noted the presence of disk material in the potential space lying between the inner and outer dural sleeves. Our patient appears to represent the first such case to be reported.
Several authors have proposed similar mechanisms by which lumbar disk herniation results in transdural migration of a disk fragment.[4,7,19] Although unclear, the pathogenesis is thought to be the result of tight adhesions between the ventral dura and the posterior longitudinal ligament (PLL). According to this model, as the nucleus herniates it penetrates the annulus, PLL, and dura, all of which are closely adherent and act as a single fibrous layer. Hlavin and Hardy suggest that these adhesions also serve as a barrier to lateral migration of the fragment, forcing it directly dorsal through the annulus-PLL-dural layer.[7] This model is supported by the dense adhesions found between the dura and PLL in autopsy studies. The strength of the adhesions appears to vary by vertebral level.
The presence of tight PLL-to-dural adhesions in the lumbar spine is most common at L4-5 followed by L3-4 and L5-S1.19 Smith reported clinical correlations of these autopsy findings.[16] The frequency of intradural disk herniation was greatest at L4-5 followed by L3-4. Outside the lumbar region, the most common levels to be affected by intradural disk herniation are T9-10, T10-11, and C5-6.
Based on the proposed model, how can sequestration of a herniated disk fragment between the inner and outer dural sleeves be explained? One hypothesis is that the disk fragment only partially migrates through the dura without sufficient force to penetrate the inner dural layer. Perhaps transdural migration of the interdural disk fragment would be complete with time. In our patient, the time between symptom onset and surgery was only 5 weeks. Conversely, more than 80% of the reported cases with intradural disk fragments had been symptomatic for more than a year,[8] and many of the remaining cases had symptoms for more than 2 months. These findings seem to support the theory that interdural sequestration may simply be an intermediate stage in the process of complete transdural migration of a disk fragment.
A final issue to be considered is the enhancement of the disk fragment on MR imaging. Enhancement of herniated disk material is relatively common. However, the issue is less clear when intradural fragments are considered, primarily because of the rarity of the event itself. In several reports, intradural disk herniation has been associated with fragment enhancement on MR imaging.[6,10,18] When enhancement occurs, the likelihood of confusing the disk material with a neoplastic lesion becomes even greater. Histopathologic examination then becomes crucial for diagnosis.
Conclusion
This case represents the first report of histopathologically confirmed herniated disk sequestration between the inner and outer dural sleeves. The pathogenesis of this condition is unclear but may be related to tight PLL-to-dural adhesions. Surgeons must be aware of this condition when confronted with an MR image suggestive of an intradural extramedullary neoplastic process.
References
- Akdemir H, Oktem I, Koc K, et al: Postoperative intraradicular lumbar disc herniation. A case report. Neurosurg Rev 20:71-74, 1997
- Alonso-Bartolome P, Canga A, Vazquez-Barquero A, et al: Intradural lumbar disk herniation [Spanish]. Neurologia 16:181-184, 2001
- Bayassi S: Intradural lumbar disk herniation (ILDH): Case report and literature review [Polish]. Neurol Neurochir Pol 32:1295-1301, 1998
- Dandy WE: Serious complications of ruptured intervertebral discs. JAMA 11:474-475, 1942
- Fang CM, Huang TJ, Chen WJ, et al: Intradural lumbar disc herniation–A case report. Changgeng Yi Xue Za Zhi 17:297-300, 1994
- Hida K, Iwasaki Y, Abe H, et al: Magnetic resonance imaging of intradural lumbar disc herniation. J Clin Neurosci 6:345-347, 1999
- Hlavin ML, Hardy RW, Jr.: Lumbar disc disease. Neurosurg Quart 1:47, 1991
- Kataoka O, Nishibayashi Y, Sho T: Intradural lumbar disk herniation: Report of three cases with a review of the literature. Spine 14:529-533, 1989
- Koc R, Akdemir H, Oktem I, et al: Intradural lumbar disc herniation: Report of two cases. Neurosurg Rev 24:44-47, 2001
- Lidov M, Stollman A, Casden A, et al: MRI of lumbar intradural disc herniation. Clin Imaging 18:173-178, 1994
- Mut M, Berker M, Palaoglu S: Intraradicular disc herniations in the lumbar spine and a new classification of intradural disc herniations. Spinal Cord 39:545-548, 2001
- Nazzal MM, Croissant PD, Ali MA, et al: Intraradicular disc herniation: A case report and review of the literature. J Spinal Disord 8:86-88, 1995
- Prestar FJ, Schattke HH: Intradural lumbar disc herniations: A report of three cases. Minim Invasive Neurosurg 38:125-128, 1995
- Reina GE, Calogne ER, Heriot RM: Transdural lumbar disc herniation. Spine 19:617-619, 1994
- Schisano G, Franco A, Nina P: Intraradicular and intradural lumbar disc herniation: Experiences with nine cases. Surg Neurol 44:536-543, 1995
- Smith RV: Intradural disc rupture. Report of two cases. J Neurosurg 55:117-120, 1981
- Suzer T, Tahta K, Coskun E: Intraradicular lumbar disc herniation: Case report and review of the literature. Neurosurgery 41:956-958, 1997
- Whittaker CK, Bernhardt M: Magnetic resonance imaging shows gadolinium enhancement of intradural herniated disc. Spine 19:1505-1507, 1994
- Yildizhan A, Pasaoglu A, Okten T, et al: Intradural disc herniations. Pathogenesis, clinical picture, diagnosis and treatment. Acta Neurochir (Wien) 110:160-165, 1991
