Choroid Plexus Mimicking Posterior Fossa Hemangioblastoma in a Patient with von Hippel-Lindau Syndrome
Harry H. Gebhard, MD*
Iman Feiz-Erfan, MD
Peyman R. Tabrizi, MD**
L. Fernando Gonzalez, MD
Robert F. Spetzler, MD
Division of Neurological Surgery, Barrow Neurological Institute, St. Joseph’s Hospital and Medical Center, Phoenix, Arizona
*Ludwig-Maximilians University, Munich, Germany
Current Address: **Western Medical Center, Santa Ana, CA
Abbreviations Used: MR, magnetic resonance
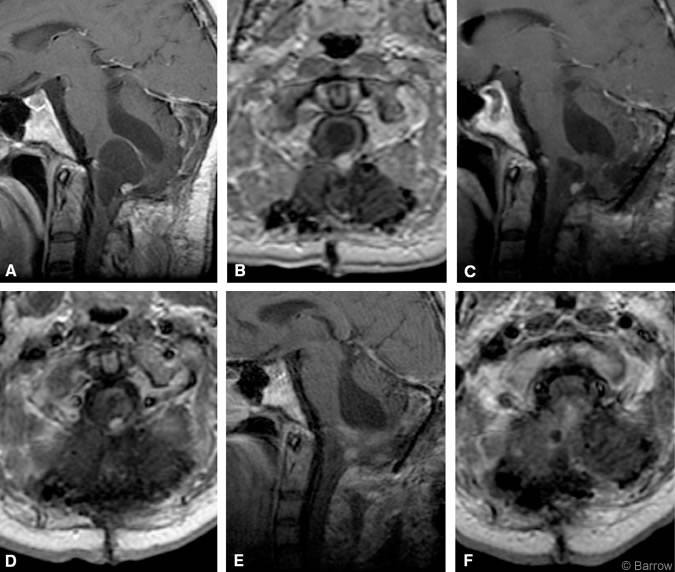
On MR imaging, hemangioblastomas of the central nervous system typically appear as cystic lesions with an enhancing mural nodule. A 42-year-old man with known von Hippel-Lindau syndrome was admitted to our institution for progressive ataxia and dysphagia. MR imaging showed a cystic lesion with an enhancing nodule located in the dorsal medulla oblongata associated with significant mass effect (Panels A and B).
Earlier, the patient had undergone four midline suboccipital craniotomies for resection of a hemangioblastoma in the inferior vermis and region of the fourth ventricle. On this occasion, a midline suboccipital approach was performed with frameless neuronavigation, and the cystic lesion was identified. At surgery resected tissue was thought to represent a hemangioblastoma, but histological analysis did not confirm this clinical and radiological diagnosis. The tissue was described as fibrotic and gliotic without evidence of neoplasia. Postoperatively, the patient developed the new onset of cardiogenic syncope, which was treated with a transitory cardiac pacemaker. Postoperative MR imaging (Panels C and D) showed significant reduction in the size of the cyst and enhancing nodule.
To prevent further cardiac decline related to progression of the lesion, the patient underwent another procedure 2 weeks later to resect the lesion, which, clinically, was still considered to represent a hemangioblastoma. The same approach was performed again with the aid of frameless neuronavigation. Intraoperatively, the nodule appeared to be a loop of choroid plexus outside the confines of the fourth ventricle, which was the only structure matching the intraoperative neuronavigational data. The nodule was resected and choroid plexus was confirmed by histological analysis. Residual cystic fluid was drained. Postoperative enhanced MR imaging (Panels E and F) confirmed the absence of the enhancing nodule and decompression of residual cystic fluid. Two weeks after this procedure, the patient’s preoperative ataxia and dysphagia had improved significantly. His cardiogenic dysfunction also was improving steadily.
We believe that a loop of choroid plexus likely became misplaced and walled off from the cerebrospinal fluid pathways when scar tissue formed in response to the patient’s repeated surgeries. The resulting focal cyst formation and compression mimicked a hemangioblastoma in our patient with von Hippel-Lindau syndrome.