Endoscopic Spine Surgery
Overview
Endoscopic spine surgery uses an endoscope (for example, the joimax® endoscopic spine solution)—a thin, flexible tube with a light and small camera at the end—to visualize and repair problems like a herniated disc or pinched nerve through a tiny incision, often measured in millimeters. With endoscopic spine surgery, surgeons can precisely access and treat spinal conditions through these small incisions, reducing the trauma to nearby tissues.
Endoscopic spine surgery can help address a range of spinal conditions, including a herniated disc, spinal stenosis, and chronic back pain. It also supports a range of spinal neurosurgery procedures and minimizes postoperative pain, recovery time, and scarring.
Did you know?
Endoscopes can vary in size, from miniature to standard, and even include a capsule endoscope that travels through the digestive tract like a pill.
Steps of Endoscopic Spine Surgery
Endoscopic spine surgery procedures typically involve the following steps:
- A small incision—often less than 1 inch long—is made near the affected area of the spine.
- The surgeon inserts a guide to navigate to the affected area using natural anatomical pathways, such as the corridors between different muscles.
- The endoscope is inserted along this path to provide a magnified view of the surgical area, enhancing surgical precision.
- Specialized micro-instruments are passed through the endoscope to remove herniated disc material, decompress nerves, remove or repair damaged tissue, or perform other interventions.
- Once the procedure is complete, the neurosurgeon removes the instruments and endoscope, and the incision is closed with minimal suturing.
Using small incisions and precise paths, endoscopic spine surgery helps minimize damage to surrounding tissue, often resulting in faster recovery, less postoperative pain, and a reduced need for time under general anesthesia.
In fact, the endoscopic spine surgery significantly reduces muscle damage because it eliminates the need for muscles and ligaments to be pulled back from the operating space. This minimally invasive surgery also dramatically reduces recovery time compared to traditional spine surgery.

What can endoscopic spine surgery treat?
Endoscopic spine surgery is designed to treat various spinal conditions, particularly those that cause back and leg pain due to nerve compression.
Neurosurgeons commonly use it to address:
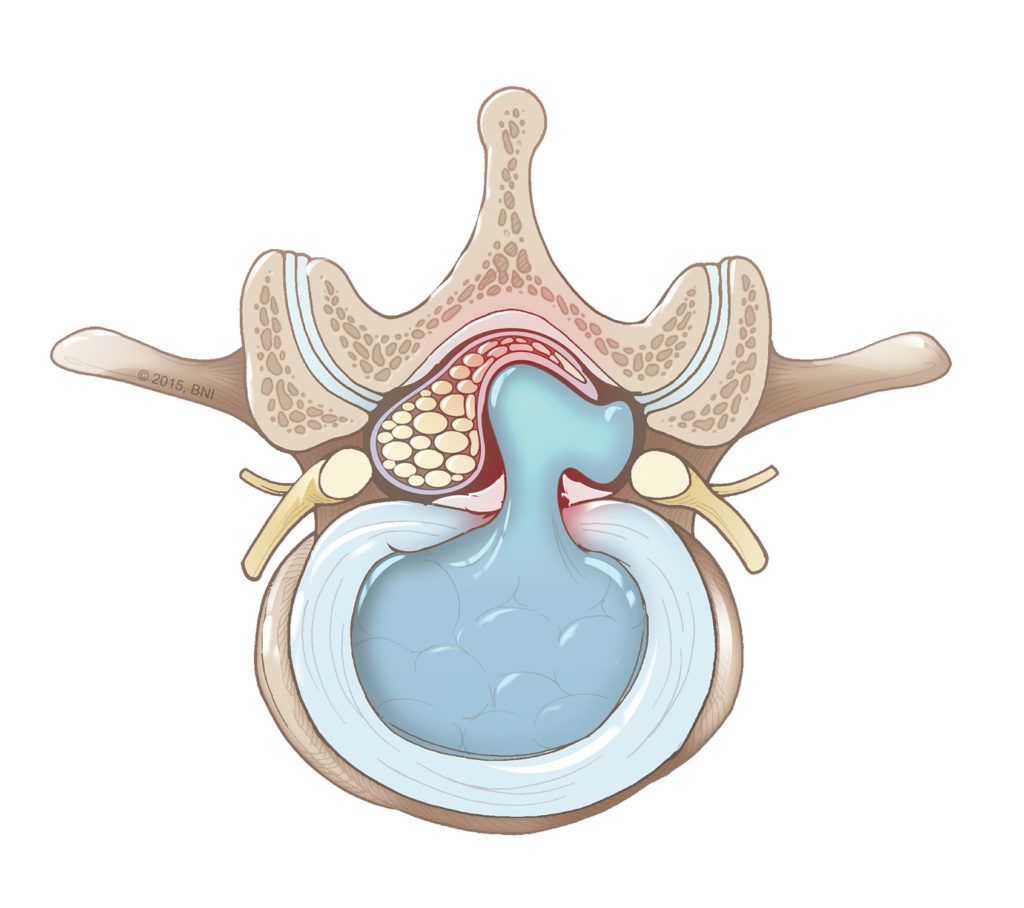
- Herniated discs: Not all patients with a herniated disc require surgery, but your spinal neurosurgeon may recommend endoscopic surgery if nonsurgical treatments have been ineffective.
- Spinal stenosis: When the spaces within the spinal canal in the lower back narrow, pressure can build up on spinal nerves, requiring surgery to restore space around the affected nerves.
- Degenerative disc disease: If spinal discs wear down over time from degenerative disc disease, endoscopic surgery can help stabilize and repair the damaged discs.
- Facet joint cysts: Endoscopic surgery can remove cysts that form in the spine’s facet joints and compress nearby nerve roots.
- Chronic back or leg pain: When structural issues cause chronic back or leg pain, endoscopic surgery can be offered as a viable treatment.
- Failed back surgery syndrome (FBSS): When previous procedures haven’t relieved back pain or associated symptoms, your doctor may recommend endoscopic revision surgery.
- Spine tumors: In select cases, a minimally invasive approach to a biopsy or spinal tumor removal can be done using endoscopic spine surgery.
Common Questions
How often is endoscopic spine surgery performed?
Endoscopic spine surgery is becoming more common. The joimax system used at Barrow is among the most widely used systems in endoscopic spine surgery in the U.S. and around the world. In fact, a study published in World Neurosurgery found that 36.5 percent of surveyed spine surgeons have relied on this system.
Are there any risks associated with endoscopic spine surgery?
While endoscopic spine surgery is generally considered safe, risks and potential complications are still associated with its use, as with any surgical procedure. These can include:
- Bleeding: Minor bleeding can occur, especially if a blood vessel is damaged during the surgical procedure.
- Infection: Any surgical incision carries some risk of infection, though the risk is reduced compared to traditional open surgery.
- Nerve injury: Since the surgery involves operating near spinal nerves, there’s a small risk of temporary or permanent nerve damage, which could cause numbness, weakness, or pain.
- Dural tear: Accidental puncture of the protective covering of the spinal cord, called the dura, may lead to cerebrospinal fluid leaks and require additional treatment.
- Incomplete relief of symptoms: In some cases, the procedure may not fully resolve pain or mobility issues, or symptoms may return.
- Need for further surgery: If the initial procedure doesn’t achieve the desired result or complications arise, revision surgery may be needed.
When used by trained spine surgeons, endoscopic spine surgery is associated with lower complication rates than traditional open spine surgery.
What kind of results can I expect with endoscopic spine surgery?
Patients undergoing endoscopic spine surgery can expect favorable outcomes, especially when used for conditions like herniated discs.
Results will often include:
- A shorter recovery time: Because the procedure is minimally invasive, most endoscopic spine surgery patients can return to light activities within a few days and resume regular routines within a few weeks.
- Reduced pain: Many patients report significant relief from back or leg pain shortly after the procedure, often within days.
- Minimal scarring: Due to the small incisions used by endoscopic spine surgery systems, scarring is minimal.
- Lower complication rates: Compared to traditional open surgery, there is a lower infection risk, less blood loss, and a reduced need for pain medications after the procedure.
- Higher patient satisfaction: Studies and patient surveys report high satisfaction rates due to the quicker recovery, reduced pain, and fewer postoperative limitations.
That said, the effectiveness of endoscopic spine surgery procedures will vary, depending on your condition, how long you’ve had symptoms, your overall health, the experience of your spine surgeon, and your age. In rare cases, you may need additional procedures if symptoms persist or recur.
Physical therapy can also be a key component in recovery following an endoscopic spine surgery procedure. Engaging in physical therapy after minimally invasive spine surgery helps reduce pain, strengthen the muscles around the spine, and enhance recovery.